THE MOVEMENT DIAGRAM; GEOFF’S HERITAGE, DOES IT HIT THE NAIL ON THE HEAD?
The movement diagram; Geoff Maitland’s heritage, does it hit the nail on the head? (if you double click on the inserted images you will find the enlarged version, this should facilitate reading)
I would like to start of with a quote from Maitland’s peripheral manipulation fourth edition edited by the late Kevin Banks and Elly Hengeveld 2005; “The movement diagram is intended solely as a teaching aid and as a means of communication, It is intended to help newcomers in the method of manual examination and makes them analyse the movement in terms like range, pain, resistance and protective spasm and makes them (intended as the newcomers) analyse the manner in which these factors interact to affect the movement. Movement diagrams and also the grades of movement are not necessarily essential to using passive movements as a form of treatment. However they are essential to understanding the relationship that the various grades of movement have to a patient’s abnormal joint signs”.
Traditionally pain as a symptom and resistance behavior have been explained and related to biological, structural, mostly “joint” related biomechanical and “orthopedic “ aspects and views of the human movement born in an early era’s up until the mid 90-ies. The mid 90-ies were kind of a starting point where many of the once so proudly presented “diagnostic”, “structural” views based on morphological and biomechanical changes shared by several health care providers started to make place for current, more science based, more “holistic”, partially philosophical views on human movement and on suffering.
Alternative explanations for pain had been around much earlier than the mid 90-ies, for example Patrick Wall’s pain mechanism; a new theory in 1965, the puzzle of pain in 1974 and the challenge of pain in 1982 had been introducing aspects of the ascending and descending central nervous system in pain behavior.
The dominant biological model of the human body had to make place for other models integrating psycho-emotional, psychosocial, philosophical and many other aspects, like general physical condition, sleep patterns, gut health, life style and many many other factors that are directly or indirectly related to pain and suffering… this massive and in a way “revolutionizing” body of evidence trying to understand “the pain puzzle” is ongoing!
IMTA is dealing with this current and constant flow of research findings and following the discussions regarding relevance and integration of research findings in our daily practice.

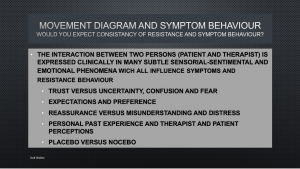
This means that patients reactions to treatment are highly individual and related to many, some maybe known but also many unknown factors intertwining constantly and determinating treatment and it’s loadability.
“Knowledge is a subset of that what is both true and believed” the Theaetetus, Plato’s dialogue concerning the nature of knowledge… 369 BC.
Geoff Maitland’s heritage is without doubt important; patient centeredness, clinical reasoning, clinical decision making based on a hypothetical deductive model, progression of treatment and continuous reassessment are known to be cornerstones in rehabilitation but unfortunately also subject to potential individual and group related bias, therefore attention to potential reasoning pitfalls and bias requires a constant internal critical view.
For me reason to drop a critical look on the use of the movement diagram. Can the movement diagram be used in a clinical decision making process? Can it decide on where to treat, how to treat, in which directions to tread and can it help in making decisions on how to dose the treatment?
My intention is to share my reflections, presenting thoughts and some of the studies affiliated to the subject and to stimulate a discussion on an intellectual level.
Decision making processes related to aspects influencing treatment modalities in daily practice should never be based on single factors, we all know that.
It is very hard to believe that physiotherapists are able to produce similar movement diagrams, that a movement diagram can be helpful to come to similar treatment decisions since many non modifiable factors play a major role.
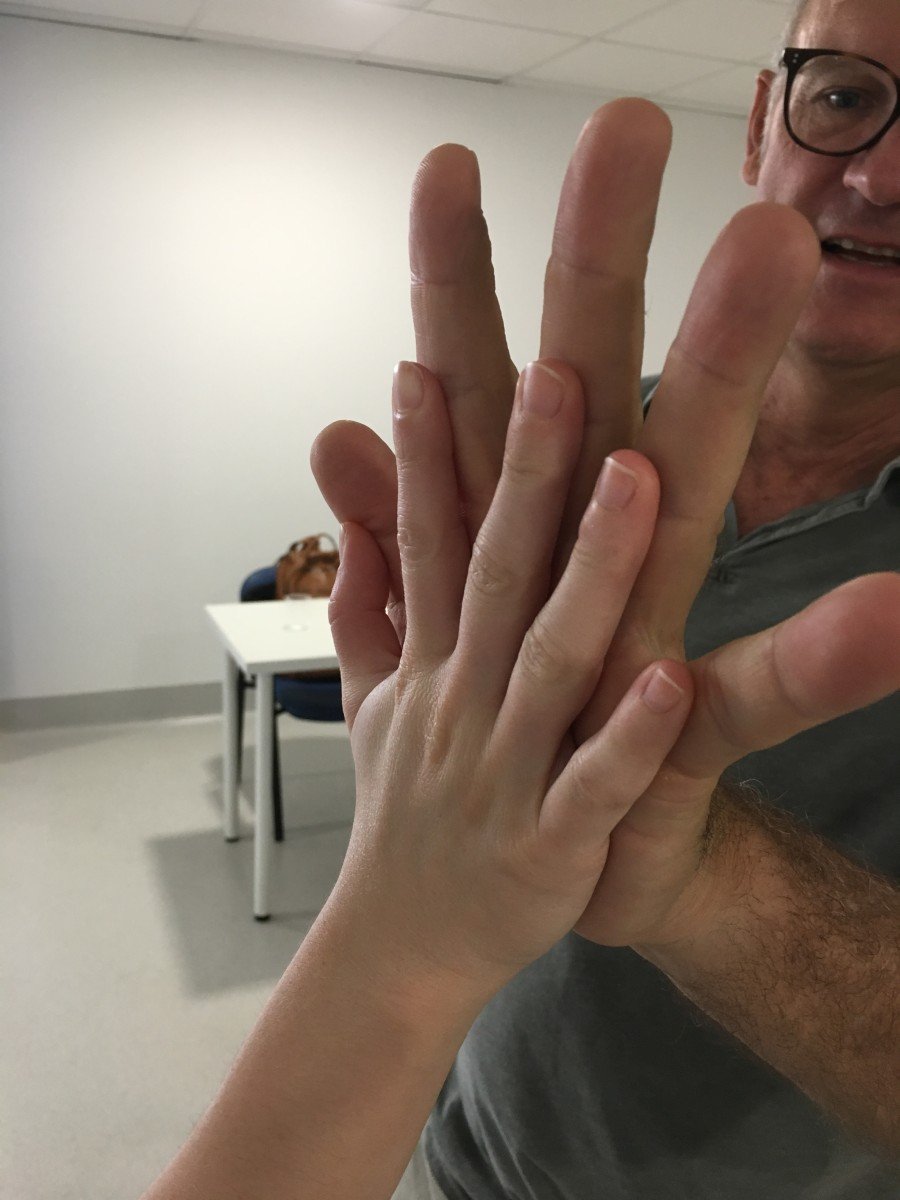
I am not the biggest fella around (1.82 Mtrs and 84 Kg) but I would not expect to find the same elements of resistance behavior and pain behavior as compared to many of my colleagues and not only for weight and height reasons!
I have to admit that I never have been a great “fan” of the movement diagram although I do partially recognize it’s role as an “educational tool” in the starting phase of learning. I obviously also do recognize that in some situations the examination of altered movement can be expressed as “limited” or “restricted” with or without loss of functionality and on the other side of the movement spectrum movement can be judged as abundant but functional, or maybe even abundant and momentarily not “fit” enough to guarantee full desired function, in need of more indicated strategies to recover, if possible, ideal function.
"Students apply lower forces than therapists" (48). Similar factors were associated with applied forces for both groups: male gender and greater subject body weight were associated with higher applied forces, and greater C2 stiffness with lower forces. Having thumb pain was associated with lower applied forces for therapists but higher ones for students.Experienced physiotherapists apply greater force than physiotherapy students across all grades, despite similar oscillation frequency. the experienced physiotherapists applied a maximum force that was almost 50% higher than the force applied by the students
In one study (38), patients with low back pain were randomly assigned to one of three groups i) Lumbar manipulations ii) Placebo manipulations iii) Placebo manipulations with a re-assuring sentence, “The manual therapy technique you will receive has been shown to significantly reduce low back pain in some people”. All 3 groups had similar immediate and 2-week outcomes with respect to pain and disability. However, the patients receiving the placebo MT with the simple re-assuring sentence had the greatest level of satisfaction with their treatment
It is easy for clinicians to perceive the benefits seen following the application of any MT to be directly the result of the MT technique. However a meta-analysis shows us that as little as 3% of pain relief can be attributed to the actual MT treatment and the rest can be attributed to natural history, patient motivation and expectations maximized by re-assurance,(36).
I’ve always had though this “gut feeling” that frequently the movement diagram had elements which I considered far too much “subjective”, related to far too many different factors other than strictly “the tissues” and that decision making processes related to the movement diagram gave an “illusion of precision”. Besides that, some of the delayed post treatment clinical features like pain and protective stiffness are not expressed in a movement diagram before treatment or while under treatment but rather as an delayed reaction after treatment and will need treatment adaptation’s and maybe alternative rehabilitation strategies for sure.
Can palpation and the analytical use of the movement diagram be of help in finding the location where to treat? Or better said does the most painful or most restricted joint needs to be treated?
"Manual therapists commonly use assessments of intervertebral motion to determine the need for spinal manipulation, but the reliability of these procedures demonstrates conflicting results". The objectives of this study (41) were to investigate the interrater reliability of thoracic spine motion palpation for perceived joint restriction and pain. Methods. Twenty-five participants between the ages of 18 and 70, with or without mid-back pain, were enrolled. Two raters motion palpated marked T5–T12 levels using two methods (standardised and pragmatic) and noted any restricted or painful segments. We calculated agreement between two raters by generating raw agreement percentages and Kappa coefficients with 95% confidence intervals. Results. There was poor to low level of agreement between the raters for both joint stiffness and pain localization using both pragmatic and standardized approaches. The results did not improve significantly when we conducted a post hoc analysis where three spinal levels were collapsed as one and right and left sides were also combined. Conclusions. The results for interrater reliability were poor for motion restriction and pain. These findings may have unfavourable implications for all manual therapists who use motion palpation to select patients appropriate for spinal manipulation.
The above mentioned studies speak clear… this means that the decision making process in musculoskeletal physiotherapy on where to treat and how to treat is under “discussion”. There may be many ways to deal with pain and treatment need to address varies aspects of the patient’s problem… I’am sure we all agree on that.
Movement diagram features are maybe part of a decision making process but it’s elements “resistance behavior” and symptom behavior” are prone to play a far too important role in decision making and have to be put into a larger bio-psycho-social model and that larger picture has to pass right from the very start of an educational process.
Another feature which I find “hard to accept” is the fact that in some of the publications of the movement diagram pain is found to be around before resistance arrives.
I would expect resistance R1 to be at least together with the arrival of P1.. Discussions on where and how to define R1 have been published (34)
There could be some advantage in treating pain with some degree of pain provocation. It opens up the interesting option in observing the patient’s capacity of endogenous pain modulation therefore testing the patient’s supraspinal mechanisms of pain modulation.
Emerging evidence supports the hypothesis that MT produces a non-specific neurophysiological effect that may better explain the modulation of pain and muscle tone via the central nervous system (CNS) (5,6) (Bialosky et al 2013, Bialosky et al 2009. The inhibition of nociception has been proposed to occur at the periaqueductal gray (PAG) and the rostroventral medulla (RVM) of the CNS (Bialosky et al 2011).
So, maybe it it is enough to ask ourselves the next simple questions?
But passive treatment, if expected to be in the patient’s interest, can be delivered in many different ways and is not necessarily related to the application of one single set of treatment parameters… I am sure many of you already build in the following.
By the way, as far as treatment precision is concerned, and since active movement is a vital part of rehabilitation processes, what parameters do you use in active rehabilitation? How do you decide whether a patient is generally fit enough to deal with ADL? What are your tests which decide on general condition? How do you follow-up and progress the initially chosen parameters? How do you dose your training as far as aerobic/anearobic exercise is concerned? When is someone ready to return to sports related activity and return to play? Do you use heart rate variability as a parameter to monitor physical condition in your patients? What are your parameters when you have to deal with active resistance training or strength training? How do you start a training program for persons suffering from persistent pain? These are just a few of the many questions every physiotherapist dealing with patients has to ask herself (himself) every single day in trying to analyze and optimize the many relevant factors involved in rehabilitation.
So… you may think that you hit the nail on the head, using the movement diagram, certainly it’s your choice, but you have to know it’s intrinsic restrictions and limitations as far as judgements of normal and abnormal, as supposed to finding the “right segment” or the “right dosis” and the “right movement direction” for treatment. I do believe that the movement diagram is an educational tool in some way… “but don’t hit that nail too hard!”
1. Abbott JH, Flynn TW, Fritz JM, Hing WA, Reid D, Whitman JM. Manual physical assessment of spinal segmental motion: intent and validity. Man Ther. 2009 Feb;14(1):36-44.
2. Aquino RL, Caires PM, Furtado FC,. Applying Joint Mobilization at Different Cervical Vertebral Levels does not Influence Immediate Pain Reduction in Patients with Chronic Neck Pain: A Randomized Clinical Trial. J Man Manip Ther. 2009 Apr 1;17(2):95–100.
3. Bialosky JE, Bishop M, George S, Placebo response to manual therapy: something out of nothing? J Man Manip Ther. 2011 Feb;19(1):11–9.
4. Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The Mechanisms of Manual Therapy in the Treatment of Musculoskeletal Pain: A Comprehensive Model. Man Ther. 2009 Oct;14(5):531–8.
5. Bialosky JE, et al. Spinal manipulative therapy-specific changes in pain sensitivity in individuals with low back pain. J Pain. 2014 Feb;15(2):136-48.
6. Bialosky JE, Bishop M, George S, Placebo response to manual therapy: something out of nothing? J Man Manip Ther. 2011 Feb;19(1):11–9.
7. Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The Mechanisms of Manual Therapy in the Treatment of Musculoskeletal Pain: A Comprehensive Model. Man Ther. 2009 Oct;14(5):531–8
8. Bialosky JE, George SZ, Horn ME, Price DD, Staud R, Robinson ME. Spinal manipulative therapy-specific changes in pain sensitivity in individuals with low back pain. J Pain. 2014 Feb;15(2):136-48.
9. Bible JE(a), Biswas D, Miller CP, Whang PG, Grauer JN. Normal functional
range of motion of the lumbar spine during 15 activities of daily living. J Spinal
Disord Tech. 2010 Apr;23(2):106-12.7. Bible JE(b), Biswas D, Miller CP, Whang PG, Grauer JN. Normal functional range of motion of the cervical spine during 15 activities of daily living. J Spinal Disord Tech. 2010 Feb;23(1):15-21.
10. Bible JE(b), Biswas D, Miller CP, Whang PG, Grauer JN. Normal functional range of motion of the cervical spine during 15 activities of daily living. J Spinal Disord Tech. 2010 Feb;23(1):15-21.
11. Chaudhry H, Schleip R, Ji Z, Bukiet B, Maney M, Findley T. Three-Dimensional Mathematical Model for Deformation of Human Fasciae in Manual Therapy. JAOA J Am Osteopath Assoc. 2008 Aug 1;108(8):379–90.
12. Childs JD, Fritz JM, Flynn TW, Irrgang JJ, Johnson KK, Majkowski GR, Delitto A. A clinical prediction rule to identify patients with low back pain most likely to benefit from spinal manipulation: a validation study. Ann Intern Med. 2004 Dec 21;141(12):920-8.
13. Chiradejnant A, Maher CG, Latimer J, Stepkovitch N. Efficacy of “therapist- selected” versus “randomly selected” mobilisation techniques for the treatment of low back pain: a randomised controlled trial. Aust J Physiother. 2003;49(4):233- 41.
14. Cleland JA, Childs JD, McRae M, Palmer JA, Stowell T. Immediate effects of thoracic manipulation in patients with neck pain: a randomized clinical trial. Man Ther. 2005 May;10(2):127– 35.
15. Coughlin AM1, Badura AS, Fleischer TD, Guck TP. Multidisciplinary treatment of chronic pain patients: its efficacy in changing patient locus of control. Arch Phys Med Rehabil. 2000 Jun;81(6):739-40.
16. de Oliveira RF, Liebano RE, Costa LC, Rissato LL, Costa LO. Immediate effects of region-specific and non-region-specific spinal manipulative therapy in patients with chronic low back pain: a randomized controlled trial. Phys Ther. 2013; 93: 748– 75
17. Donaldson M, Petersen S, , et al A Prescriptively Selected Non-Thrust Manipulation Versus a Therapist Selected Non-Thrust Manipulation for Treatment of Individuals With Low Back Pain: A Randomized Clinical Trial. J Orthop Sports Phys Ther. 2016 Mar 8:1-29.
18. Dunning J, Mourad F, Barbero M, Leoni D, Cescon C, Butts R. Bilateral and multiple cavitation sounds during upper cervical thrust manipulation. BMC Musculoskelet Disord. 2013 Jan 15;14:24.
19. Flynn TW, Fritz JM, Wainner RS, The audible pop is not necessary for successful spinal high-velocity thrust manipulation in individuals with low back pain. Arch Phys Med Rehabil. 2003 Jul;84(7):1057–60.
20. Gagnon D.H. et al, Do experienced physiotherapists and final year physiotherapy trainees apply similar force during posterior-to-anterior lumbar mobilization techniques? Manual Therapy xxx (2015) 1-5
21. Gross AR, Goldsmith C, Hoving JL, Haines T, Peloso P, Aker P Conservative management of mechanical neck disorders: a systematic review. J Rheumatol. 2007 May;34(5):1083-102. Epub 2007 Jan 15.
22. Haneline MT, Young M. A review of intraexaminer and interexaminer reliability of static spinal palpation: a literature synthesis. J Manipulative Physiol Ther. 2009 Jun;32(5):379-86.
23. Hayes MA1, Howard TC, Gruel CR, Kopta JA. Roentgenographic evaluation of lumbar spine flexion-extension in asymptomatic individuals. Spine (Phila Pa 1976). 1989 Mar;14(3):327-31.
24. Hegedus EJ, Goode A, Butler RJ, Slaven E. The neurophysiological effects of a single session of spinal joint mobilization: does the effect last? J Man Manip Ther. 2011; 19: 143– 151.
25. Hestbaek L, Leboeuf-Yde C. Are chiropractic tests for the lumbo-pelvic spine reliable and valid? A systematic critical literature review. J Manipulative Physiol Ther. 2000 May;23(4):258-75.
26. Hicks GE, Fritz JM, Delitto A, McGill SM. Preliminary development of a clinical prediction rule for determining which patients with low back pain will respond to a stabilization exercise program. Arch Phys Med Rehabil. 2005 Sep;86(9):1753- 62.
27. Huijbregts PA. Spinal Motion Palpation: A Review of Reliability Studies. J Man Manip Ther. 2002 Jan1;10(1):24–39.
28. Huisman PA, Speksnijder CM, de Wijer A. The effect of thoracic spine manipulation on pain and disability in patients with non-specific neck pain: a systematic review. Disabil Rehabil. 2013 Sep;35(20):1677–85
29. Johnson AJ, Godges JJ, Zimmermann GJ, Ounanian LL. The effect of anterior versus posterior glide joint mobilization on external rotation range of motion in patients with shoulder adhesive capsulitis. Journal of Orthopaedic and Sports Physical Therapy 2007;37(3):88–99
30. Keedy NH, Keffala VJ, Altmaier EM1, Chen JJ. Health locus of control and self- efficacy predict back pain rehabilitation outcomes. Iowa Orthop J. 2014;34:158-65.
31. Landel R, Kulig K, Fredericson M, Li B, Powers CM. Intertester reliability and validity of motion assessments during lumbar spine accessory motion testing. Phys Ther. 2008 Jan;88(1):43–9.
32. Maher C, Adams R. Reliability of pain and stiffness assessments in clinical manual lumbar spine examination. Phys Ther. 1994 Sep;74(9):801–809; discussion 809–811.
33. Maitland GD: Vertebral Manipulation, ed 5. Butterworth & Co, London, 1986
34. Maitland GD: peripheral manipulation, ed 4. Elsevier, 2005
35. Melzack R Evolution of the neuromatrix theory of pain. The Prithvi Raj Lecture: presented at the third World Congress of World Institute of Pain, Barcelona 2004. Pain Pract. 2005 Jun;5(2):85-94.
36. Menke JM. Do manual therapies help low back pain? A comparative effectiveness meta-analysis. Spine. 2014 Apr 1;39(7):E463–47
37. Mulligan BR. Manual Therapy, NAGS, SNAGS, MWMS. Plane View Services, Wellington, New Zealand 1999
38. Nyberg RE, Russell Smith A. The science of spinal motion palpation: a review and update with implications for assessment and intervention. J Man Manip Ther. 2013 Aug;21(3):160–7.
39. Petty N. et al, Manual examination of accessory movements–seeking R1. Manual Therapy (2002) 7(1), 39–43
40. Pattyn E, Rajendran D2. Anatomical landmark position–can we trust what we see? Results from an online reliability and validity study of osteopaths. Man Ther. 2014 Apr;19(2):158-64.
41. Ross JK, Bereznick DE, McGill SM. Determining cavitation location during lumbar and thoracic spinal manipulation: is spinal manipulation accurate and specific? Spine. 2004 Jul 1;29(13):1452– 7.
42. Rubinstein SM, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW. Spinal manipulative therapy for acute low back pain: an update of the cochrane review. Spine (Phila Pa 1976). 2013 Feb 1;38(3):E158-77.
43. Schomacher J. The Effect of an Analgesic Mobilization Technique When Applied at Symptomatic or Asymptomatic Levels of the Cervical Spine in Subjects with Neck Pain: A Randomized Controlled Trial. J Man Manip Ther. 2009 Apr 1;17(2):101–8.
44. Schroeder J, Kaplan L, Fischer DJ, Skelly AC. The outcomes of manipulation or mobilization therapy compared with physical therapy or exercise for neck pain: a systematic review. Evid Based Spine Care J. 2013 Apr;4(1):30-
45. Seffinger MA, Najm WI, Mishra SI, Adams A, Dickerson VM, Murphy LS, et al. Reliability of spinal palpation for diagnosis of back and neck pain: a systematic review of the literature. Spine. 2004 Oct 1;29(19):E413–425.
46. Seffinger, M.A., King, H.H., Ward, R.C., Jones, J.M. III, Rogers, F.J., Patterson, M.M. Osteopathic philosophy. in: R.C. Ward (Ed.) Foundations for osteopathic medicine. 2nd ed. Lippincott Williams & Wilkins, Philadelphia, PA; 2003:3–18.
47. Slater SL1, Ford JJ, Richards MC, Taylor NF, Surkitt LD, Hahne AJ. The effectiveness of sub-group specific manual therapy for low back pain: a systematic review. Man Ther. 2012 Jun;17(3):201-12.
48. Snodgrass S. at al, A Comparison of Cervical Spine Mobilization Forces Applied by Experienced and Novice Physiotherapists, journal of orthopaedic & sports physical therapy, volume 40, number 7, 2010
49. Stovall BA, Kumar S. Anatomical landmark asymmetry assessment in the lumbar spine and pelvis: a review of reliability. J Am Osteopath Assoc. 2010 Nov;110(11):667-74
50. Sutlive TG, Mabry LM, Easterling EJ, Durbin JD, Hanson SL, Wainner RS, Childs JD. Comparison of short-term response to two spinal manipulation techniques for patients with low back pain in a military beneficiary population. Mil Med. 2009 Jul;174(7):750-6.
51. Threlkeld AJ. The effects of manual therapy on connective tissue. Phys Ther. 1992 Dec;72(12):893–902.
52. Tullberg T, Blomberg S, Branth B, Johnsson R. Manipulation does not alter the position of the sacroiliac joint. A roentgen stereophotogrammetric analysis. Spine. 1998 May 15;23(10):1124-8
53. Young JL, Walker D, Snyder S, Daly K. Thoracic manipulation versus mobilization in patients with mechanical neck pain: a systematic review. J Man Manip Ther. 2014 Aug;22(3):141-53.
54. Walker B.F. et al, Interrater Reliability of Motion Palpation in the Thoracic Spine, Evidence-Based Complementary and Alternative Medicine
Volume 2015 (2015), Article ID 815407




Comments