Musculoskeletal Pain and PNEI considerations
Musculoskeletal Pain and
Bio-Psycho-Neuro-Endocrine-Immune interplay
Rolf Walter
The biological, tissue based model:
Diagnosis as well as management of musculoskeletal pain and dysfunction is traditionally leaning heavily on tissue associated or biological models although around up to 77% of case scenarios are reported as having potential diagnostic inaccuracies in a systematic review due to personality traits, cognitive issues, anchoring, confirmation and availability biases (Saposnik et al 2016).
Despite availability of concurrent reasoning models research suggests that physiotherapists continue to focus on tissue related aspects. Analysis suggests that, in general, physiotherapy training mostly is guided by ‘’established expectations’’ of what a physiotherapist ‘should’ focus on, and institutional circumstances strongly draw the attention of physiotherapists towards biological aspects (Mescouto et al 2022).
Traditional manual therapy models are based on mobility testing of ‘’joint related’’ problems (Van Trijffel et al 2010) and several derivates of that traditional model can be found within proposed educational clinical reasoning models and flowcharts like the component model below.
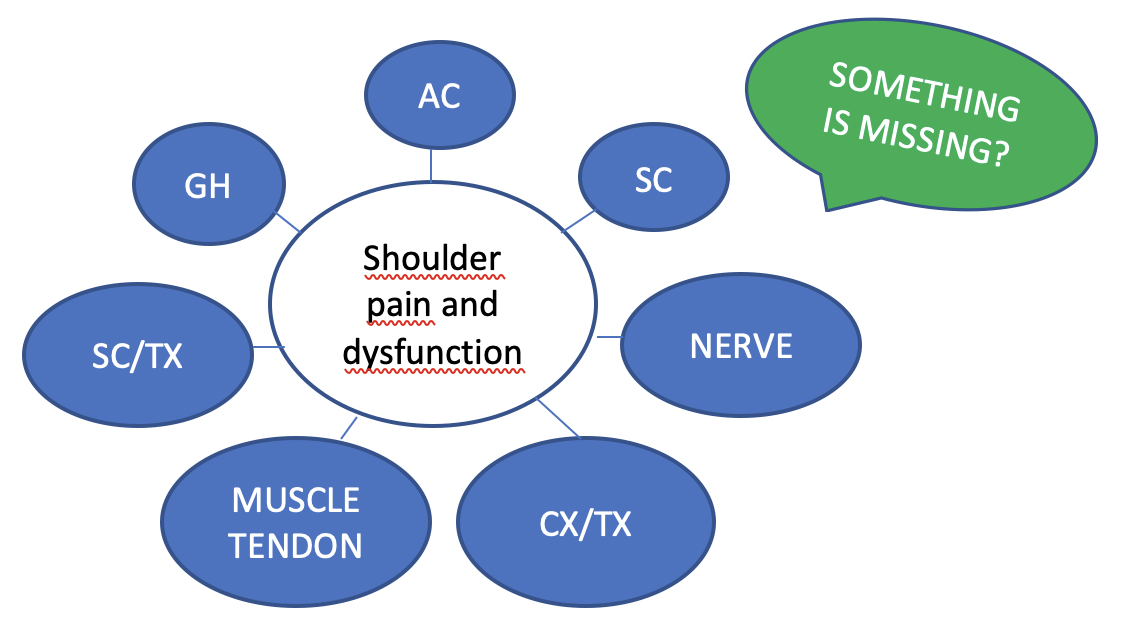
Obviously there is, in itself, nothing wrong with using ‘’tissue based models’’, ‘’tissue based problems’’ exist in some of our patients but unsurprisingly, and as we all know and acknowledge reasoning all too often stops right there. The percentage of accuracy as well as the relevance of ‘’tissue based’’ diagnosis and models is though being questioned as they show elevated amounts of false positives in imaging as well as in clinical examinations. Positive pain provocation tests are not per definition reliable and accurate in diagnostic testing as extensively shown in Chad Cook’s and Eric Hegedus’ book on orthopedic testing. Also positive cluster testing may not be as accurate as previously thought (Saueressig et al 2021, Salahm et al 2020). False positives, or frequent, daily fluctuations of sensitivity on testing may occur. Changing symptom and signs before and after treatment testing may are frequently observable but the interpretation as well as the consistency of the symptomatic tests used may fluctuate considerably in some patients as dependent of the individuals amount of inflammatory process; interleukin-1 b, substance P and cytokines as well as circadian symptom fluctuations in anxiety disorders, post-traumatic stress disorders, obsessive-compulsive disorders menstrual cycle (Green et al 2022). Several other scenario’s are being explained later in this blog. So provocation, modification and modulation of signs and symptoms can be used as parameters in a hypothetic-deductive concept, but may lack consistency and the interpretation should be done with great care and certainly not solely in a tissue based model. We all see patients who show us inconsistency of obtained results, unexplainable flutuations of signs and symptoms
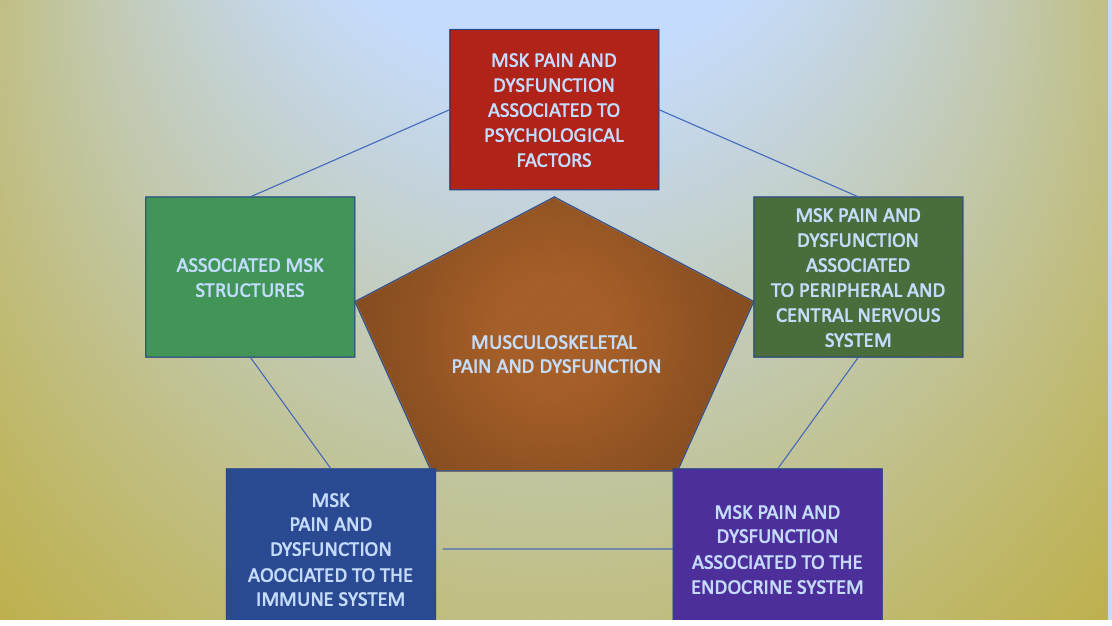
Posttraumatic, post-surgical local and systemic inflammation are not two separate entities and you cannot ‘’shut off’’ the controlling psycho-neuro-endocrine-immunology ‘’background systems’’ involved in inflammatory processes constantly regulating body homeostasis and metabolism (Klyne et al 2021). Some of our patients will show massively delayed recovery after trauma or surgery, disrespecting the considered ‘’normal physiological timeline’’ of tissue recovery. The models we use reflect our reasoning processes.
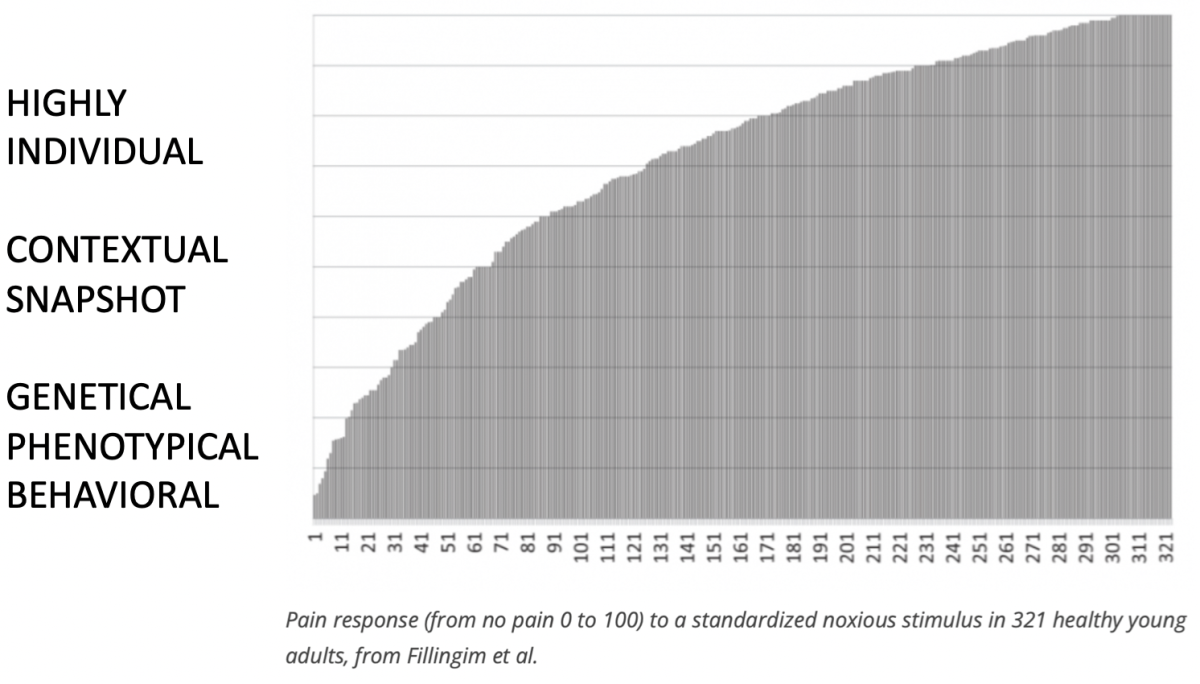
In the Maitland concept, we not only uses tissue based reasoning models, IMTA embraces also more holistic models like the bio-psycho-social model and pain related models like the input-elaboration-output model or ‘’mature organism’’ model by the late Louis Gifford. The ‘’mature organism’’ model as well as other explanations, in vogue in pain related publications have been though under scrutiny of several researchers in the pain field and accused of being far too much ‘’brain centered’’. So, discussions and challenges around the issue pain are more intense and controversial now than ever, new discoveries that feed discussions are emerging at high speed. Lets put it this way, it’s not the right time to fanatically support strong opinions on any kind of pain theory or specific opinions shared by groups with vested interests on the topic of pain. That begs the question.. where is pain science heading, what is there in store, is there an ultimate answer to the discussion? Fact is that pain responses to sensory stimulation are extremely individual as shown by Fillingim et al. Definitely clinically observable in our patients.
‘’sensory stimulation is necessary but not sufficient for pain’’
‘’sensory stimulation may lead to pain but the amount of pain is dependent on the persons, highly individual, sensory treshold’’
There is a need for clear indications for the choice of conservative, best evidence informed NMSK management. The decision making around best practice should not depend on the practitioners favorite technique, application, vested interests or exercise but depend on the best available evidence based/patient centered choice. The same best available evidenced advice you would expect from your medical doctor on NMSK surgical management or if you need medication. We all appreciate that decision making in the medical field is not that easy. We all see patients on a rather regular base where medical management has led to adverse effects.
I personally believe that there is, if indeed indicated, a place for manual examination as well as for some form of manual care in the process of rehabilitation. I also don’t think even that manual care will ever be completely abandoned as possible integrative part within rehabilitation processes, nor I do believe that it is a ''wise action'' to abandon ''hands on'' care. If I do use manual care as part of overall NMSK care in patients I use the reasoning models that are intergrative part of NMSK therapy. I do though strongly support the current process of reflection, discussions and publications on the theme of modernization and on the topic of ‘’hands on’’ and ‘’hands of’’ care.
In a vast percentage of my patients hands on management is simply not indicated, like not all patients who go to surgeons for an opinion should get surgery. As said, that doesn’t mean that there is also a group of patients who might profit of some hands on care besides other modalities of care, as well as there are patients who seek non other than manual care and that may lead to management problems in itself. Again, we need indications for our choices of the correct and evidence supported choice of modalities. In the absence of a clear history of a provoking event, and that is the case in the majority of my patients, the question should be. ‘’ what are the elements feeding the patients problem’’?.
There was and is a reason why we currently prefer to speak about neuro-musculoskeletal management instead of manual therapy management since the wording used simply either broadens or narrows the reasoning processes as well as the choice towards (preferred?) management options.
If we have a broad-based analytical look at our patients we cannot deny that there potentially is a rather large spectrum of diversity, btw extensively tackled in the IMTA webinar I did a couple of years ago. The vulnerability we may encounter in some of our patients seems to have no limit and is definitely not only related to physical or tissue related vulnerability, there is a massive body of evidence that shows that various vulnerability models exist and that various systems are involved in vulnerability (Delgado-Sanchez et al 2023).
Let us first reflect on what epidemiological data say on general population, that may give a lead as to where I want to go with this blog. Around 30% of general population will have some form of sensory sensitivity, an individual, genetically influenced trait, not related to a specific age but associated with greater depth of information processing, a lowering of sensory threshold and an ease towards overstimulation, therefore a neurophysiological event at the basis of neural sensitization and thus correlated with pain (Acevedo et al 2014, Koechlin et al 2023). I guess that those were the patients Geoff Maitland referred to as ‘’jointy people’’.
First off all I have substantial doubt that we as practitioners see an equal distribution of sensory sensitivity (30%) of the general population in our clinics since the population we tend to see has been pre-selected, in most cases, by medical practitioners. A substantial percentage of those patients gets a biological, tissue based medical diagnosis which may carry an emotional load and lead to unnecessary suffering in some patients. The medical diagnosis may not completely cover the potentially complex psycho-neuro-endocrine-immunological factors they suffer from that influence their overall health, physical dysfunction as well as NMSK related pain. We may assume that there is a substantial risk that the sensory sensitivity percentage rates in our clinics maybe be quite a bit higher as I am not aware of any existing publication who deals with the question.
The evaluation of the bodily sensation of pain, on the other hand, is called suffering and is related to past experience, meaning, social influences, psychological traits, context and maybe also to cultural influences and leads to behavioral output, emotional reactions and behavioral sensitization (Klein C. 2015). Pain is a sensation whilst suffering is the perception, pain is not the same as suffering.
‘’Suffering is an emotional response,
suffering can be with pain or without pain’’
‘’So, pain is not the same as suffering’’
Despite the substantial differences between the various systems that are involved in psycho-neuro-endocrine-immunology (PNEI) they influence each other strongly in their mutual role in trying to maintain homeostasis during the entire human lifespan (Hachmeriyan et al 2022). PNEI is always involved, for the good as well as a disturbing factor. PNEI systems are involved in local as well as systemic inflammatory processes (Klyne et al 2021),
But PNEI related factors in MSK pain and dysfunction may be less obvious, partially hidden, not well understood and therefore not recognized although these factors may influence management, prognosis, expectations and outcome. If you observe the following features in your patients you might want to think of disturbing systemic factors:
no clear history of onset of their symptoms and suffer symptom fluctuations over time spans
- pain episodes without consistent onset, physical dysfunctions which show inconsistency or episodes of physical dysfunctions,
- short lived or inconsistent treatment results, sudden unexplainable worsening or improvements
- stress, anxiety, depression or in general mindset related pain
- sleep disorders
- overweight and metabolic disorders
- gut and stool disorders related to long lasting back pain possibly related to lower back Modic 1 changes
- monthly cyclic painful episodes in women, circadian fluctuations of pain
- development of MSK disorders after menopause
- pain which is not clearly movement or position related or symptom inconsistency over time
- nutrition related pain
- general health issues, comorbidities
- skin related signs and symptoms
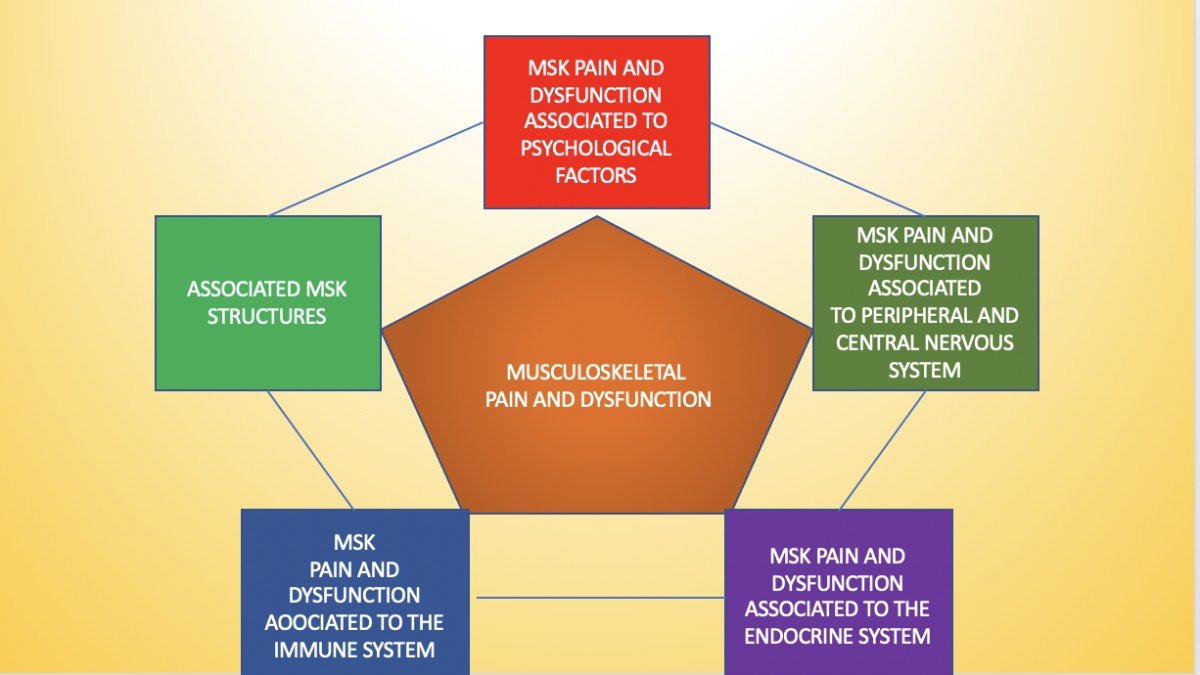
Below follows a series of, for the purpose of this blog selected number of factors and details which purpose it is to highlight and sensitize the reader to the different PNEI systematic influences on MSK pain and dysfunction:
- Your endocrine system is a bidirectional message system, it has a neuro-endocrine part as well as a gland related part that regulates the speed of all important, physiological processes of our body inherent to body metabolism, homeostasis (Hironori et al 2023), psychological wellbeing and all other vital body functions (Plunk et al 2020).
- your gut is an endocrine organ, is involved in various psychological pathologies (Lie et al 2023), depression (Liu et al 2023) low back pain (Geng et al 2023), osteoporosis, sarcopenia, rheumatoid arthritis, anchylosing spondylitis as well as fractures (Dekker Niter M. 2020)(Chen S. 2023) and is part of a gut-brain bi-directional axis. Your gut micriobiome interacts bidrectionally with drug inntake and determines drug toxicity of commonly used drugs (Weersma et al 2020)
- Depression is related to NMSK symptoms ad signs (Sapolsky 2015, Shao et al 2023, Danielson et al 2015, Hannibal et al 2015)
- Stress and emotions may elicit strong physiological and hormonal reaction that alter cognition affect and behavior (Sapolsky 2015)
- Stress activates the hypothalamus-pituitary-adrenal axis as well as several stress markers (cortisol, epinephrine, adrenaline as well as activation of the sympathetic nervous system (Shao et al 2023)
- Stress generates descending effects on biological systems and although in itself no painful may induce neurohormonal effects at the basis of diffuse pain (Hannibal et al 2014)
- A Vast body of longitudinal research has demonstrated that depression predicts future low back pain, neck and shoulder pain and in general MSK pain (Leino et al 1993 ,Croft et al 1995)
- Elevated stress can be at the basis of Crohn’s disease and ulcerative colitis (Schneider et al 2023)
- Depressive women and post-partum depression have been found to have low levels of estradiol (Holsen et al 2011)
- The neuro-endocrine system and the immune system share a common biology, stress induced neuro-endocrine changes activate the immune system (Dalacheck et al 2023)
- Body fat is an endocrine organ and excessive fat may induce low grade inflammatory processes (Coelho et al 2013) thus contributing to NMSK pain.
- Obesity is correlated with depression, metabolic syndrome, hypertension, hyperglycemia, hyperlipidemia and diabetes (Lopresti et al 2013, Martiac et al 2014)
- Body fat is part of a dynamic interactive network of metabolic, immunologic and endocrine function with significant effects on body homeostasis (Mraz et al 2014)
- Muscles are endocrine organs with immunologic, anti-inflammatory and metabolic effects thus communicating with non muscular tissues (Schnyder et al 2015, Ellingsgaard et al 2019), muscles stimulated through exercise produce exerkines (Interleukin-6, Irisin) called myokines which cross-talk with other organs like liver, pancreas, bones (osteokines), brain body fat (adipokines), neurons (neurokines), with the capacity of influencing cardiovascular health, metabolic and immune related pathologies, diabetes type 2, overweight, suppression of tumor growth and facilitation of age related general health (Chow et al 2022, Kirk et al 2020, Ellingsgaard et al 2019) Endocrine pathways involved in muscular activity influence metabolic health of your bones, liver, heart and brain and obviously also o the muscle trophism itself (Shao et al 2023)
- Muscles stimulated through exercise where high intensity exercise has more effects on myokines than moderate intensity exercise and has effects on
o BDNF (Brain Derived Neurtrophic Factor) and it’s role in neuroplasticity, brain development, memory, creative thought, depression, homeostasis, inflammatory states, obesity
o Cathepsin B, which has a vital role proteolysis of the extra cellular matrix
o Fibroblast Growth Factor—21, role in immue protection
o Follistatin Related Protein 1, cardioprotective function
- Bones are considered an endocrine organ having a role in intracellular crosstalk between neurons and MSK structures (osteokines and neurokines) and so involved in neurodegenerative diseases like Alzheimer where exercise ha shown to have positive effects (Huhaa et al 2022) osteoarthritis and osteoporosis (Schurman et al 2023), Exercise creating mechanical effects has osteogenetic properties, hormonal effects (insulin like growth effects) as well as on sexual hormones (Andrukhova et al 2016, Kajimura et al 2013)
- You nervous system is an endocrine organ, controlling pain (oxytocin, Progesteron, estrogen, pregnenolone, DHEA and gonadotropin, controlling neurogenesis and neuroplasticity (Aloisi et al 2006)
- Your heart is an endocrine organ, life style factors, stress related factors, psychological vulnerability profiles, high cholesterol levels may increase risk for myocardial infarction despite the presence of arterial health and low lipid profiles especially in females (Daniel et al 2015)
- Female hormones have less protection for pain as compared to male hormones (Maurer et al 2016, Admandusson et al 2013, Craft et al 2007, Smith et al 2002, Vincent et al 2013)
- Transgender females have indeed less pain during female to male transformation whereas the opposite, male to female transformation taking estrogens create more pain (Aloisi et al 2007, Athnaiel et al 2023)
- Hormonal fluctuations, especially female hormones may influence acute as ell as chronic pain states (Averitt et al 2019)
- Male hormones are involved in MSK pain (Tajar et al 2011)
- Intensity of symptoms is related to low levels of testosterone inn females as well as in males (Kaergaard et al, 2000, Wiholm et al 1997)
- Menopause may exacerbate NMSK signs and symptoms
- Headaches, like chronic migraines are related to complex metabolic-endocrine factors like obesity, diabetes, hypertension, metabolic syndrome, hyperthyroidism and insulin resistance (Rainero et al 2018, Fava et al 2014, Bhoi et al 2012)
- Headaches have a relationship with stress and have altered levels of glucose and insulin which contribute to metabolic disorders
It surely would take me several blogs to describe all the complex but highly interesting interactions in bio-pyscho-neuro-endorine-immunology. This blog is intended to sensitize the readers and covers only the ‘’tip of the iceberg’’. Patients with NMSK symptoms and signs are often complex. Several of my patients suffer sensory sensitivity issues, have thyroid disease, diabetes, are in the age of menopause, overweight, gut disorders as well as back pain, comorbidities like widespread pain or headaches, suffer psychological issues like fear, anxiety or depression or even psychiatric features, several of them are physically deconditioned, have sleep disorders, are in advanced age, but also adolescent pains without a history of provoking factors may have associated PNEI factors. Several of our patients will have innate or acquired sensory sensitivity issues. All in all good reason to consider alternative possible scenario’s and consider what is exactly driving the patients problem, what would be the diversified treatment modalities that may modify and improve the quality of life of your patients. Life style, stress management, information, education, relaxation, activity management, exercise and hands on management mave all have life quality influences on biological and PNEI underlying factors in NMSK pain and dysfunction.
1. Hachmeriyan A., Pashalieva I., Stefanova N., Influence of the thymus and pineal gland on immunity and aging, Scripta Scientifica Medica, 2022;54(3):15-20, doi: 10.14748/ssm.v54i2.8149
2. Saposnik G, Redelmeier D, Ruff CC, Tobler PN. Cognitive biases associated with medical decisions: a systematic review. BMC Med Inform Decis Mak. 2016 Nov 3;16(1):138. doi: 10.1186/s12911-016-0377-1.
3. Mescouto K, Olson RE, Hodges PW, et al. Physiotherapists Both Reproduce and Resist Biomedical Dominance when Working With People With Low Back Pain: A Qualitative Study Towards New Praxis. Qualitative Health Research. 2022;32(6):902-915. doi:10.1177/10497323221084358
4. Van Trijffel et al, the role and position of passive intervertebral motion assessment within clinical reasoning and decision making in manual physical therapy: a qualitative interview study, JMMT 2010
5. Acevedo B.P. et al, The highly sensitive brain; an fMRI study of sensory processing sensitivity and response to others’ emotions, Brain and Behavior 2014;4(4):580-594, doi:10.1002/brb.242
6. Koechlin H. et al, sensory processing sensitivity inn adolescents reporting chronic pain: an exploratory study, Pain reports 8, 2023
7. Klein C. What the Body Commands. Massachusetts: MIT Press; 2015.
8. Plunk E. et al, International journal of endocrinology 2020; Epigenetic Modifications due to Environment, Ageing, Nutrition, and Endocrine Disrupting Chemicals and Their Effects on the Endocrine System).
9. Hironori A. et al, Handbook of hormones, comparative endocrinology for basic and clinical research, vol 1, 2nd edition Elsevier 2023
10. Liu L., Wang H., Chen X., Zhang Y., Zhang H., Xie P., Gut microbiota and its metabolites in depression: from pathogenesis to treatment, The Lancet eBioMedicine 2023;90: 104527, https://doi.org/10. 1016/j.ebiom.2023. 104527
11. Geng Z., Wang J., Chen G., Liu J., Lan J., Zhang Z., Miao J., Gut microbiota and intervertebral disc degeneration: a bidirectional two-sample Mendelian randomization study, Journal of Orthopaedic Surgery and Research https://doi.org/10.1186/s13018-023-04081-0 (2023) 18:601
12. Dekker Niter M. et al, Altered Gut Microbiota Composition Is Associated With Back Pain in Overweight and Obese Individuals, Frontiers in Endocrinology, www.frontiersin.org 1 September 2020, Volume 11, Article 605
13. Chen S. et al, (2023) Causal effects of specific gut microbiota on musculoskeletal diseases: a bidirectional two-sample Mendelian randomization study. Front. Microbiol. 14:1238800.doi: 10.3389/fmicb.2023.1238800
14. Klyne D.M. et al, does the interaction between local and systemic inflammation provide a link from psychology and lifestyle to tissue health in musculoskeletal conditions?, IJMS, 2021
15. Delgado-Sanchez et al, Are We Any Closer to Understanding How Chronic Pain Develops? A Systematic Search and Critical Narrative Review of Existing Chronic Pain Vulnerability Models, Journal of pain research 2023
16. Cook C., Hegedus E., Orthopedic physical examination tests: an evidence based approach 2nd edition. 2011
17. Saueressig T. et al, Diagnostic accuracy of clusters of pain provocation tests for detecting sacro-iliac joint pain: systematic review with meta-analysis, 2021
18. Salahm P. et al, is it time to put special tests for rotator cuff-related shoulder pain out to pasture, JOSPT 2020
19. Green S.A. et al, Symptom fluctuations over the menstrual cycle in anxiety disorders, PTSD, and OCD: a systematic review, Arch Womens Mental Health, 2022
20. Coelho M. et al, Biochemistry of adipose tissue: an endocrine organ, Arch Med Sci 2, April / 2013
21. Liu L., Wang H., Chen X., Zhang Y., Zhang H., Xie P., Gut microbiota and its metabolites in depression: from pathogenesis to treatment, The Lancet eBioMedicine 2023;90: 104527, https://doi.org/10. 1016/j.ebiom.2023. 104527
22. Sapolsky, R. Stress and the brain: individual variability and the inverted-U. Nat Neurosci18, 1344–1346 (2015).
23. Shao R., Man I.S.C., Yau S.Y., Li C., Li P.Y.P., Hou W.K., Li S.X., Liu F.Y., Wing Y.K., Lee T.M.C., The interplay of acute cortisol response and trait affectivity in associating with stress resilience, nature mental health, vol1, 2023, 114-123
24. Danielson, C. K., Hankin, B. L. & Badanes, L. S. Youth offspring of mothers with posttraumatic stress disorder have altered stress reactivity in response to a laboratory stressor. Psychoneuroendocrinology 53, 170–178 (2015).
25. Hannibal K.E., Bishop M.D., Chronic Stress, Cortisol Dysfunction, and Pain: A Psychoneuroendocrine Rationale for Stress Management in Pain Rehabilitation
Phys Ther. Published online July 17, 2014, doi: 10.2522/ptj.20130597
26. Lopresti A.L.,et al Obesity and psychiatric disorders: commonalities in dysregulated biological pathways and their implications for treatment. Prog Neuropsychopharmacol Biol Psychiatry (2013) 45:92–9. doi:10.1016/j.pnpbp. 2013.05.005
27. Martinac M. et al, Metabolic syndrome, activity of the hypothalamic-pituitary-adrenal axis and inflammatory mediators in depressive disorder. Acta Clin Croat (2014) 53:55–71
28. Mraz M. et al, The role of adipose tissue immune cells in obesity and low grade inflammation, Journal of Endocrinology 2014, 222 R113-R127
29. Schnyder S. et al, Skeletal muscle as an endocrine organ: PGC-1α, myokines and exercise, Bone. 2015 November ; 80: 115–125. doi:10.1016/j.bone.2015.02.008
30. Ellingsgaard H. et al, Exercise and health-emerging roles of IL-6, Current opinion in physiology, 10:49-54, 2019
31. Chow L.S. et al, Exerkines in health, resilience and disease, Nature Reviews, Endocrinology, vol. 18, may 2022, 237-289
32. Kirk B. et al, Muscle, bone and fat crosstalk: the biological role of myokines, osteokines and adipokines, Springer Current Osteoporosis Research, 2020, https://doi.org/10.1007/s11914-020-00599-y
33. Shao M. et al, Advances in the research on myokine-driven regulation of bone metabolism, HELIYON (2023)
34. Huuha A.M. et al, Can exercise training teach us how to treat Alzheimer’s disease? Ageing Research Reviews 2022
35. Schurman C.A. et al, Molecular and Cellular Crosstalk between Bone and Brain: Accessing Bidirectional Neural and Musculoskeletal Signaling during Aging and Disease, J Bone Metab 2023
36. Andrukhova O. et al, Fgf23 and parathyroid hormone signaling interact in kidney and bone. Mol. Cell Endocrinol. 436, 224–239 (2016).
37. Kajimura D. et al, Adiponectin regulates bone mass via opposite central and peripheral mechanisms through FoxO1. Cell Metab. 17, 901–915 (2013).
38. Aliosi A.M. et al, Sex hormones, central nervous system and pain. Horm Behav. 2006;50:1–7.
39. Daniel M. et al, Risk factors and markers for acute myocardial infarction with angiographically normal coronary arteries. Am J Cardiol. 2015;116:838–44. doi: 10.1016/j.amjcard.2015.06.011
40. Maurer A.J. et al, pain and sex hormones: a review of current understanding, pain management 2016, doi: 10.2217/pmt-2015-0002
41. Amandusson Å. et al, Estrogenic influences in pain processing. Front. Neuroendocrinol. 34(4), 329–349 (2013).
42. Craft R.M., Modulation of pain by estrogens. Pain 132 (Suppl. 1), S3–S12 (2007).
43. Smith M.D. et al, Sex differences in hippocampal slice excitability: role of testosterone. Neuroscience 109(3), 517–530 (2002).
44. Smith M.J. et al, Effects of ovarian hormones on human cortical excitability. Ann. Neurol. 51(5), 599–603 (2002).
45. Vincent K. et al, Brain imaging reveals that engagement of descending inhibitory pain pathways in healthy women in a low endogenous estradiol state varies with testosterone. Pain 154(4), 515–524 (2013).
46. Tajar A. et al, for the European Male Aging Study Group, Elevated levels of gonadotrophins but not sex steroids are associated with musculoskeletal pain in middle-aged and older European men, Pain 2011, 1495-1501, doi: 10.1016j.pain.2011.01.048
47. Averitt D.L. et al, Role of sex hormones on pain, Oxford Research Encyclopedia of Neuroscience 2019
48. Rainero I. et al, Is migraine primarily a metaboloendocrine disorder?, Current pain and headache reports, 2018
49. Fava A. et al, Chronic migraine in women is associated with insulin resistance: a cross-sectional study. Eur J Neurol. 2014
50. Bhoi S.K. et al , Metabolic syndrome and insulin resistance in migraine. J Headache Pain. 2012;13:321–6.
51. Aloisi A.M. et al, Cross-sex hormone administration changes pain in transsexual women and men. Pain 2007.
52. Athnaiel O. et al, The role of sex hormones in pain-related conditions, Int J Mol Sci. 2023
53. Leino P. et al, Depressive and distress symptoms as predictors of low back pain, neck-shoulder pain, and other musculoskeletal morbidity: a 10-year follow- up of metal industry employees. Pain. 1993;53:89–94.
54. Croft P.R et al, Psychologic distress and low back pain. Evidence from a prospective study in the general population. Spine. 1995;20:2731–7.
55. Holsen L.M. et al. Stress response circuitry hypoactivation related to hormonal dysfunction in women with major depression. J Affect Disord (2011)
56. Dalecheck D. et al, An analysis on history of childhood adversity, anxiety, and chronic pain in adulthood and the influence of inflammatory biomarker C‐reactive protein, Scientific reports 2023
57. Kaergaard A. et al, Association between plasma testosterone and work-related neck and shoulder disorders among female workers, Scand J Work Environ Health 2000
58. Wiholm C. et al, Musculoskeletal symptoms and head- aches in VDU users - a psychophysiological study. Work Stress 1997.
59. Schneider K.M. et al, The enteric nervous system relays psychological stress to intestinal inflammation, Cell, 2023
60. Weersma R.K. et al, Interaction betwee drugs and the gut microbiome, Recent advances in basic science 2020




Comments