Post-traumatic stress symptoms and chronic pain
« Je ne sais pas ce que le passé nous réserve.» Françoise Sagan, Les faux-fuyants, 1991
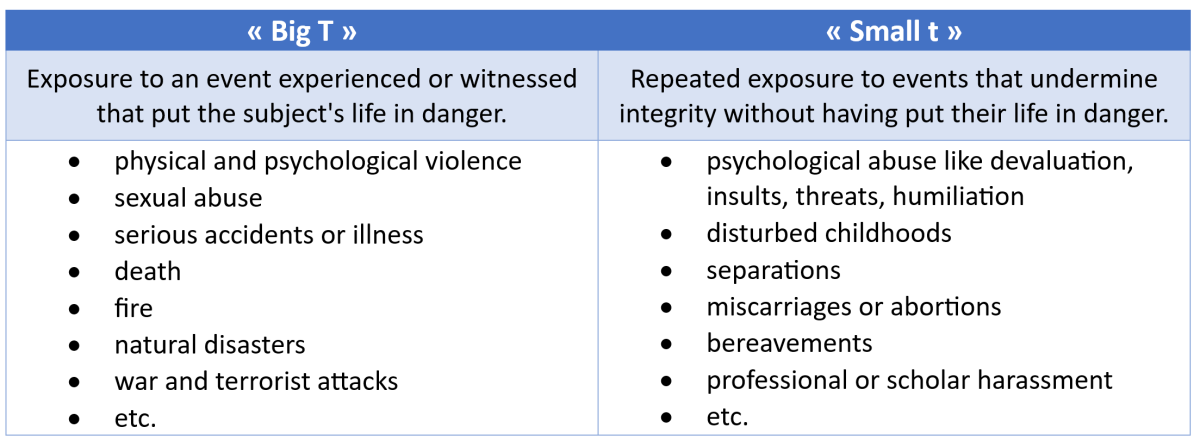
There are traumas with a small t, and Traumas with a big T. Big is evident, violent. Small can go unnoticed. None of them should be underestimated, and a small t can hide a big T.
Emotional disturbances due to traumatic experiences can interfere with human behaviour. Physiotherapists must be aware that physical symptoms can be one type of their expression in post-traumatic stress disorders (PTSD), “a psychiatric disorder that may occur in people who have experienced or witnessed a traumatic event, series of events or set of circumstances” as defined by the American Psychiatric Association.
There is a high prevalence of post-traumatic stress symptoms (PTSS) in patients suffering from chronic widespread pain, with more than 20% of them reporting higher levels of pain intensity, pain bothersomeness, disability, psychological distress, lower levels of self-efficacy, higher levels of pain catastrophizing, perceived injustice, fatigue and sleep difficulties (Linnemørken et al., 2020). Positive correlation have been observed between trauma severity and pain widespreadness, maximal pain, sleep impairment, Pain Disability Index, stress, anxiety, depression, and somatization (Manuel et al., 2023).
It is recommended to screen chronic pain patients for PTSD, since associations with central sensitization have been shown and causal relationship assumed (McKernan et al., 2019). Clinicians dealing with patients suffering from chronic pain must take this into consideration and investigate both actual and past history with increased attention to PTSS. The use of the PCL-5 is recommended in nonpsychiatric settings (Merians et al., 2023).
Cognitive behavioural therapies are first line treatments. They can be proposed in conjunction with pharmacological. Informative resources for patients can be found, among others, on the American Psychiatric Association (www.psychiatry.org).
Linnemørken, L. T. B., Granan, L.-P., & Reme, S. E. (2020). Prevalence of Posttraumatic Stress Symptoms and Associated Characteristics Among Patients With Chronic Pain Conditions in a Norwegian University Hospital Outpatient Pain Clinic. Frontiers in Psychology, 11, 749. https://doi.org/10.3389/fpsyg.2020.00749
Manuel, J., Rudolph, L., Beissner, F., Neubert, T.-A., Dusch, M., & Karst, M. (2023). Traumatic Events, Posttraumatic Stress Disorder, and Central Sensitization in Chronic Pain Patients of a German University Outpatient Pain Clinic. Psychosomatic Medicine, 85(4), 351‑357. https://doi.org/10.1097/PSY.0000000000001181
McKernan, L. C., Johnson, B. N., Crofford, L. J., Lumley, M. A., Bruehl, S., & Cheavens, J. S. (2019). Posttraumatic Stress Symptoms Mediate the Effects of Trauma Exposure on Clinical Indicators of Central Sensitization in Patients With Chronic Pain. The Clinical Journal of Pain, 35(5), 385‑393. https://doi.org/10.1097/AJP.0000000000000689
Merians, A. N., Spiller, T., Harpaz-Rotem, I., Krystal, J. H., & Pietrzak, R. H. (2023). Post-traumatic Stress Disorder. The Medical Clinics of North America, 107(1), 85‑99. https://doi.org/10.1016/j.mcna.2022.04.003
Comments
 Véronique Bornet
Véronique Bornet I would expect that most PT\'s / manual therapist will remember at least one patient in the last 10 years with expressions of PTSD.
If I look back over my career, I remember several patients who must have had post-traumatic stress, although it went unrecognized at the time. I wish sometimes that I could treat them now, as I learned more about the topic.
I remember a woman talking about an accident in which she fractured her patella. She spoke about it in such emotional detail as if it happened yesterday, but the accident was 5 years ago. I wish I had thought of asking her something as: \"how did this accident impact your life?\"or \"Does this accident haunt you?\" \"Do you dream about your accident?\" She may have more nightmares than before the accident
Another example is a man with a shoulder luxation 3 weeks ago. He was kicked off his bicycle by 3 young guys. He had severe sweating, nervousness, and eyes that could not focus for a longer period of time (got restless). My own accident left me for a while left me with some post-traumatic symptoms suas increased anxiety, palpitations, and irregular heart (all gone now with the help of a well-versed and experienced body worker/cranio sacral therapist). An 81-year golf buddy of ours, an ex-marine from the Vietnam war, recognized only 4 years ago that his inability to stay for longer periods in the same place (he moved a lot over the years after the war; always in education in US army bases of the world), nightmares and bouts of anxiety, were all expressions of a severe post-traumatic stress syndrome. He is getting help in a Veterans hospital in a specialized group. At an IFOMPT Conference in Kopenhagen, Denmark around 1996, a lecture dealt with PTSD. We were warned not to repeat the mechanisms of an accident over and over again in history-taking. (what trauma work would do, is NOT necessarily repeating the mechanisms of the incident -\"what happened\", but guiding and encouraging patients to explore what/how they felt at the time and afterwards.
I recommend readers to explore
- {{ error[0] }}