Spinal Red Flags
For too long now Physiotherapists have been asking the same standard questions to medically screen a patient. “Do you have any chest or heart problems, diabetes, epilepsy or circulatory problems?” is a common example and is often clinically irrelevant. In more recent years spinal cord compression has floated from the Orthopaedic Surgeons’ radar onto the Physio’s and therefore questions such as “any bowel or bladder problems?” have been included in our subjective examinations. However, this is still not detailed enough, because for example, a patient might not consider a symptom of serious pathology as a “problem”, if it has become their normal.
I apologise for the provocative start, but in my 34 years of clinical experience, I have seen this standardised questioning all too often.
Questioning a patient about red flags is subject to clinical reasoning as with all our questions. Therefore, the red flag questions should be personalised to each individual and should chase the appropriate hypothesis developing in the Physio’s mind, from the information gathered from each individual patient. However, developing an appropriate medical hypothesis can be our first challenge, because in medicine (and Physiotherapy) “you only see what you’re looking for and only recognise what you already know”. This is often referred to as “confirmation bias” and is based on “we see what we want to see”, because only then can we believe that we can help the patient (we need to know what we are treating to know how to treat it). So, this is why it is important to broaden our medical knowledge as much as possible, to avoid missing something we do not know about!
This even applies to some of the more obvious diagnoses, never mind the more complex and rare diagnoses. For example, up to 70% of vertebral fractures are misdiagnosed and up to 75% of spinal infections are initially misdiagnosed (Grigoryan et al 2003, McCarthy & Davis 2016). Spinal Infection is difficult to recognise clinically. In the patients I have seen with spinal infection, I knew there was something very wrong with the patient, but I didn’t know exactly what, and only appropriate investigations discovered the diagnosis. So that is also part of our role in screening, we need to know when further investigations are necessary and what investigations might be useful.
If we consider the difference between the Medical diagnosis and a Physiotherapy diagnosis, the former is trying to find the cause of the patient’s problem and as a Physio we treat the consequences of the problem. Determining the consequences is mainly based on the clinical findings, however determining the cause of a patient’s suffering is largely based on theoretical knowledge and is therefore in the realm of the Biomedical Model. So, as Physiotherapists we should work primarily in the BioPsychoSocial Model, but we still need to consider the BioMedical Model in our medical screening role.
In a nutshell, the biomedical approach can be used to screen the patient for red flags, and conditions which require early medical attention, and then the biopsychosocial approach needs to be considered to understand how the problem is affecting the patient, with a focus on the signs and symptoms rather than the structural diagnosis. As can be seen in the diagram below, red flag screening should be a priority component in the examination process, in all of our patients.
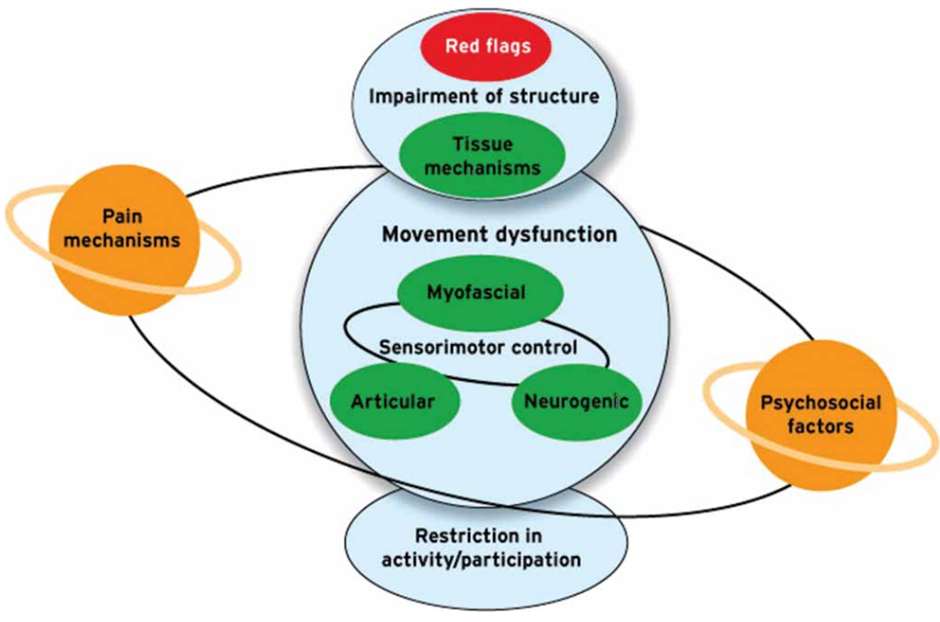
Our difficulty to establish a medical diagnosis of patients with LBP for example, has to be acknowledged, but despite all this the biomedical model still has a role in guiding decisions relating to the patients’ management, medical screening and prognosis. When considering the medical diagnosis, the patient is effectively being medically triaged and usually, this can be done via a detailed history supported by medical based examinations (blood tests, scans, etc.) rather than based on the results of any physical tests.
It is unwise to assume that if your patient has seen a Doctor prior to your appointment, that they have been medically screened already. Doctors usually have very limited time with their patients and I have many examples of patients with serious pathologies who have already seen their General Practitioner. In addition, as Physiotherapists we think very musculoskeletally, and as a result it is tempting to believe that every patient we see has a musculoskeletal problem. So, whether you work as a first contact practitioner (in the public sector in some countries and/or in the private sector in most countries) or as a secondary practitioner, red flag screening based on medical knowledge is required to ensure you are not treating a patient who should be treated elsewhere. “See the right person, at the right time, for the right treatment” (European Parliament Health Briefing 2015).
Red flags are possible indicators of serious pathology, warning signs that Physiotherapy may not be indicated, or clinical prediction guides. They should represent a clear reason for further investigation or onward medical referral.

Afterall, it is in no-one’s interest to be treating a wolf in sheep’s clothing!
The clinical guidelines for the physiotherapy management of persistent LBP (CSP, 2007) reported that there are 163 individual items that could be considered red flags for spinal pathology, 119 items in the subjective history and 44 items in the physical examination. Clearly this represents a problem in the practical clinical utility of red flags. In addition, there is a lack of good evidence to support the informativeness of the majority of red flags. Henschke et al (2013) has reported that red flags in combination have some promise, but further validation studies are required.
However, red flags are still seen as the most reliable clinical indicator for potential serious pathology and remain fundamental to our assessment process (Underwood, 2013). Because the seriousness of certain red flags warrants immediate action and others only warrant conservative observation, it is important to categorize each finding and respond based on the level of seriousness the finding poses. Some flags are more red than others!
Sizer et al (2007) categorised red flags into 3 groups:
• Category I
– Factors that require immediate medical attention
• Category II
– Factors that require subjective questioning and precautionary examination and treatment procedures
• Category III
– Factors that require further physical testing and differentiation analysis
Any red flags from category I can suggest serious pathology. These include neurological deficit not explained by a mono-radiculopathy, perianal region sensory changes, pathological changes in the bowel & bladder, non-mechanical pattern of symptoms, progressive neurological deficit and pulsatile abdominal masses.
Category II red flags include age of onset > 50 years, clonus, fever, elevated inflammatory blood tests (ESR), gait deficits, a history of a disorder with predilection of infection or haemorrhage, or a metabolic bone disorder, or cancer, long term corticosteroid use, non-healing sores or wounds and a recent history of unexplained weight loss.
A single category II red flag might not warrant concern however, the more red flags you identify in a patient, the more your index of suspicion should rise. Certain clusters of red flags also need consideration; a patient with LBP with an age of onset over 50 years and whom is on long term steroids has a dramatically increased chance of a spinal compression fracture. According to Jarvik et al (2002) a patient with a failure of previous conservative treatment + unexplained weight loss + a history of cancer + age 50+ = a sensitivity of nearly 100% for identifying a malignancy.
Category III red flags include abnormal reflexes, bilateral or unilateral radiculopathy or paraesthesia, unexplained referred pain, and unexplained significant upper or lower limb weakness.
In addition, there are non-specific red flags such as a clinical presentation which differs from known clinical patterns, no treatment response (better or worse), and symptom behaviour over time which does not match the prognosis. Any of these clinical occurrences should prompt you to think about a possible non mechanical condition, that may require further medical investigations and/or interventions.
With regards to serious spinal aetiologies, the most common 4 to consider are cauda equina syndrome, fracture, benign or malignant lesions, and infection. Early recognition of serious pathology depends on awareness, vigilance and suspicion rather than rules (Grieve, 1994). Awareness comes from increasing our medical knowledge and vigilance is related to our detail of questioning and examination of each patient. As most of the red flags are in the subjective examination then our vigilant questioning of each patient is essential.
Cauda Equina Syndrome (CES):

Unfortunately, there are no broadly accepted definitive diagnostic criteria for CES. Fraser et al (2009) identified 17 different definitions! Our diagnostic challenge is further compounded by the fact that the initial signs and symptoms are often subtle and vague, varying in intensity and progression. Only by careful, detailed history taking and examination of the patient, can CES be diagnosed early and therefore treated early to avoid life-long disability (Ma et al, 2009).
Of all the red flags listed in relation to CES there are 5 key characteristics which are consistently described in the literature and therefore should form the basis of your questions related to diagnosis. These are bilateral neurogenic sciatica, reduced perineal sensation, painless bladder retention, loss of anal tone and a loss of sexual function. The level of evidence for all these signs and symptoms on their own, is LOW. So again, you have to rely on clinical judgement and consider the whole picture, and the more significant findings are made the more your index of suspicion should rise. History and timescale are important. If all the changes are recent then urgent referral maybe necessary.
Greenhalgh et al in 2018, advised on a little more detail to our bowel and bladder questioning to help screen for CES. They advised on 3 important screening questions:
Vital Question 1: Have you noticed any numbness or strange sensations around your buttocks or between your legs? Does the toilet paper feel normal when you wipe your bottom?
Vital Question 2: Has your bladder been working normally? Can you tell when it’s full? Have you had any loss of control (accidents) or difficulty passing urine? Or have you felt that you want to go all the time?
Vital Question 3: Have you experienced any unusual problems with your bowels recently? Have you noticed any changes in sexual function, like a loss of feeling in your genitals or not being able to get an erection or ejaculate?
If CES is suspected then all the literature agrees on an urgent medical opinion and intervention, therefore a referral to the emergency department is appropriate. Early surgical decompression is essential which has a large amount of supporting literature, but there is contention around timing – many authors say surgery is optimal within 48 hours (from the onset of bowel or urinary dysfunction) for a good recovery. Therefore, although early diagnosis is difficult, if you have any suspicions, it is better to be safe than sorry and refer asap. “Nothing is to be gained by delaying surgery and much can be lost” (Germon et al, 2015).
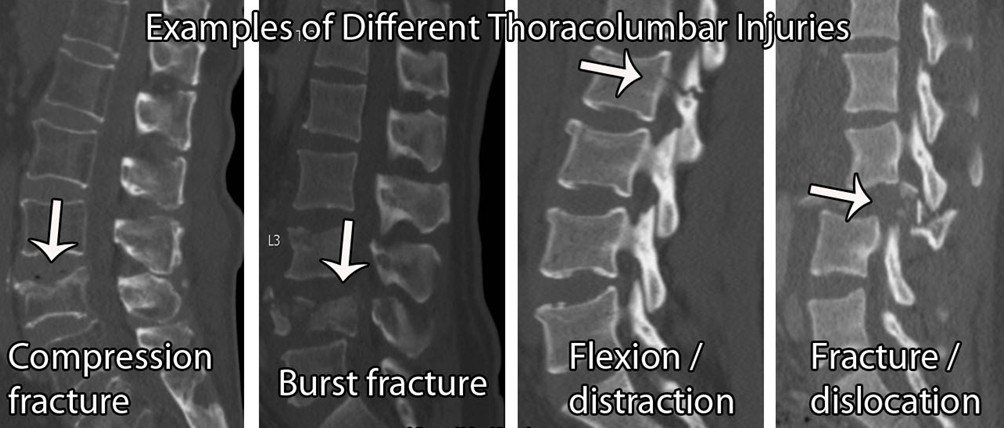
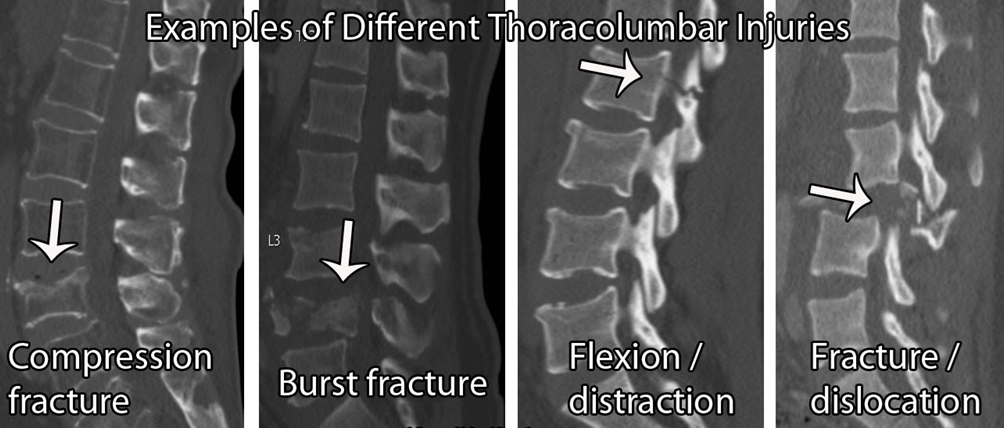
Spinal Fracture:
Generally, the red flags for diagnosing vertebral fractures are unhelpful. There are many false positives, with a low diagnostic accuracy (Williams et al 2013). So, if fracture is suspected, it is important to question your patient about the broader risk factors.
The risk factors for bone weakening include; excess alcohol (≥ 3 units per day), vitamin D deficiency, long term steroid use (≥5mg/day over 3 months), rheumatoid arthritis, diabetes, smoking ( ≥ 20/day), dietary restrictions, eating disorders, absorption problems e.g. Crohn’s disease. Now again, the level of evidence for most of these on their own is low and therefore, the more positive findings you get, the more suspicious you are.
If a patient presents in your clinic with a sudden onset of thoracic or lumbar pain, then a fracture should be on your list of suspects. This hypothesis would be further supported if the patient has a history of previous osteoporotic fractures, other osteoporotic risk factors (as above), a past history of cancer, known osteoporosis or myeloma, midline bony tenderness, and/or an onset over 65 in females or over 75 in males.
Spinal Malignancy:

After spinal fracture, metastatic bone disease is the 2nd most common serious spinal condition. Spinal bone metastases are common from cancers of the breast, bronchus/lung, thyroid, kidneys and prostate. Again, the bad news is that there are no red flags specific for spinal malignancy, therefore we must consider the red flags for cancer generally.
These include:
Pain with minimal relief (constant/constant and at night), but be aware that some cancer pain is eased by medications and pain is not always an early presentation,
Previous history of cancer,
An age of onset > 50 years old, or less than 20 years old
Fatigue, systemically unwell,
Weight loss (up to 5-10% of body weight over 3-6 months, Nicholson et al 2019), but note weight loss is not always a factor, especially in the early stages.
When screening for malignancy in LBP patients, a systematic review by Henschke et al in 2007, found the most useful features and tests are a previous history of cancer, an elevated ESR, reduced haematocrit, and clinical judgement. The only factor with a high level of evidence, is the previous history of the cancers with a predilection to metastasize.
The presence of metastases in the spine could progress to metastatic spinal cord compression (MSCC). From the 163 red flags, none are specific to MSCC. The challenge for us is that it is difficult to diagnose, and early diagnosis is very important because, delays in diagnosis and treatment can lead to paraplegia and double incontinence.
Turnpenney et al (2013) produced a list of early warning signs for MSCC, which we should consider as the basis for our red flag questioning:
Referred back pain multi-segmental or band like,
Escalating pain, poor response to treatment,
Different character or site to previous symptoms,
Funny feelings, odd sensations, or heavy legs,
Lying flat increases the back pain,
Agonising pain causing anguish & despair,
Gait disturbance, unsteadiness, esp. on stairs,
Sleep grossly disturbed with pain worse at night.
Any combination of these red flags should increase your suspicion and the more red flags, the higher the risk and the greater the urgency to refer the patient on for medical aid.
Spinal Infection:

Spinal infection refers to any infectious disease of the spinal structures e.g. the vertebrae, the discs, or the adjacent paraspinal tissues. Again unfortunately, spinal infection is difficult to recognise clinically. In high income and upper middle-income countries, the rate of infection has steadily increased, possibly due to an increasing ageing population and increased intra-venous drug use. In low-income countries it’s also increased, maybe due to HIV/Aids and tuberculosis (TB) epidemics (Lener et al, 2018).
When considering a spinal infection, it is again important to question the patient appropriately, which would entail screening for the associated risk factors (Yusuf et al, 2019).
These include:
Immunosuppressant comorbidities such as diabetes, long term steroid use, smoking, HIV/AIDS;
Social factors such as intravenous drug use, obesity, and a family history of TB;
Environmental factors such as living conditions (overcrowded, homeless, imprisonment), and the country of birth (born in a TB-endemic country);
Previous spinal surgery.
All the evidence for red flags indicating spinal infection individually, are of a low level. So again, the more red flags you find the more your level of suspicion should rise, and you have to rely to some degree on clinical judgement. The questions that need to be asked and screened in the subjective examination are the constancy of the pain (C/C), high intensity pain, sudden onset, fever, chills, sweats, skin rash (Herpes zoster), fatigue, malaise, unexplained weight loss, recent surgery or infection (last 4 weeks) and night pain (>60 minutes to settle).
The time between the onset of an infection and the diagnosis is often prolonged. Patients can be relatively healthy until symptoms manifest in the later stages. The progression is commonly more linear (malignancy progression can wax and wane). Of the infection triad (spinal pain, fever and neurological dysfunction), LBP is the most common symptom, which can progress to neurological symptoms. However, many people don’t present with all 3, only 50% of patients report a fever (Lener et al 2018). Therefore, the absence of a fever cannot rule out a spinal infection. Untreated progression can lead to paralysis, spinal instability and fatality. So, as with all these conditions, it is worth noting that a failure to refer a patient on as necessary, is a form of doing harm to the patient, which is something our screening of red flags is trying to prevent.
Conclusion:
The prevalence of serious spinal pathologies is rare, with the literature quoting from 1% (Wilk, 2004) to 14.8% (Street et al, 2020). However, we can quickly see 100 patients with LBP and a few of those might have a sinister cause and need to be anywhere else but in your clinic. Therefore, clinicians need to be able to identify patients who will require medical intervention and our best chance of achieving this is with appropriate, clinically reasoned, detailed questioning.
Good Luck and Best Wishes,
Matthew

References:
Finucane, L. M., Downie, A., Mercer, C., Greenhalgh, S. M., Boissonnault, W. G., Pool-Goudzwaard, A. L., Beneciuk, J. M., Leech, R. L., & Selfe, J. (2020). International Framework for Red Flags for Potential Serious Spinal Pathologies. Journal of Orthopaedic & Sports Physical Therapy, 50(7), 1–23. https://doi.org/10.2519/jospt.2020.9971
Fraser, S., Roberts, L., & Murphy, E. (2009). Cauda Equina Syndrome: A Literature Review of Its Definition and Clinical Presentation. Archives of Physical Medicine and Rehabilitation, 90(11), 1964–1968. https://doi.org/10.1016/j.apmr.2009.03.021
Germon, T., Ahuja, S., Casey, A. T. H., Todd, N. V., & Rai, A. (2015). British Association of Spine Surgeons standards of care for cauda equina syndrome. The Spine Journal, 15(3), S2–S4. https://doi.org/10.1016/j.spinee.2015.01.006
Greenhalgh, S., Finucane, L., Mercer, C., & Selfe, J. (2018). Assessment and management of cauda equina syndrome. Musculoskeletal Science and Practice, 37, 69–74. https://doi.org/10.1016/j.msksp.2018.06.002
Grieve, G. P. (1994). Grieve’s modern manual therapy : the vertebral column. 2nd Edition. Churchill Livingstone.
Grigoryan, M., Guermazi, A., Roemer, F. W., Delmas, P. D., & Genant, H. K. (2003). Recognizing and reporting osteoporotic vertebral fractures. European Spine Journal, 12(0), S104–S112. https://doi.org/10.1007/s00586-003-0613-0
Henschke, N., Maher, C. G., & Refshauge, K. M. (2007). Screening for malignancy in low back pain patients: a systematic review. European Spine Journal, 16(10), 1673–1679. https://doi.org/10.1007/s00586-007-0412-0
Henschke, N., Maher, C. G., Ostelo, R. W., de Vet, H. C., Macaskill, P., & Irwig, L. (2013). Red flags to screen for malignancy in patients with low-back pain. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd008686.pub2
Jarvik, J. G., & Deyo, R. A. (2002). Diagnostic Evaluation of Low Back Pain with Emphasis on Imaging. Annals of Internal Medicine, 137(7), 586. https://doi.org/10.7326/0003-4819-137-7-200210010-00010
Lener, S., Hartmann, S., Barbagallo, G. M. V., Certo, F., Thomé, C., & Tschugg, A. (2018). Management of spinal infection: a review of the literature. Acta Neurochirurgica, 160(3), 487–496. https://doi.org/10.1007/s00701-018-3467-2
Ma, B., Wu, H., Jia, L., Yuan, W., Shi, G., & Shi, J. (2009). Cauda equina syndrome: a review of clinical progress. 122(10), 1214–1222.
McCarthy J, Davis A. (2016). Diagnosis and Management of Vertebral Compression Fractures. Am Fam Physician. Jul 1;94(1):44-50. PMID: 27386723.
Nicholson, B. D., Aveyard, P., Hamilton, W., & Hobbs, F. D. R. (2019). When should unexpected weight loss warrant further investigation to exclude cancer? BMJ, l5271. https://doi.org/10.1136/bmj.l5271
Scholz, N., (2015). Personalised medicine: The right treatment for the right person at the right time EPRS | European Parliamentary Research Service; Members' Research Service PE 569.009
Sizer, P. S., Brismée, J.-M., & Cook, C. (2007). Medical Screening for Red Flags in the Diagnosis and Management of Musculoskeletal Spine Pain. Pain Practice, 7(1), 53–71. https://doi.org/10.1111/j.1533-2500.2007.00112.x
Street, K. J., White, S. G., & Vandal, A. C. (2020). Clinical prevalence and population incidence of serious pathologies among patients undergoing magnetic resonance imaging for low back pain. The Spine Journal, 20(1), 101–111. https://doi.org/10.1016/j.spinee.2019.09.002
Turnpenney, J., Greenhalgh, S., Richards, L., Crabtree, A., & Selfe, J. (2013). Developing an early alert system for metastatic spinal cord compression (MSCC): Red Flag credit cards. Primary Health Care Research & Development, 16(01), 14–20. https://doi.org/10.1017/s1463423613000376
Underwood, M., Buchbinder, R. (2013). Red flags for back pain. BMJ, 347: f7432.
Wilk, V. (2004). Acute low back pain: assessment and management. Australian Family Physician, 33(6), 403–407.
Williams, C. M., Henschke, N., Maher, C. G., van Tulder, M. W., Koes, B. W., Macaskill, P., & Irwig, L. (2013). Red flags to screen for vertebral fracture in patients presenting with low-back pain. Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.cd008643.pub2
Yusuf, M., Finucane, L., & Selfe, J. (2019). Red flags for the early detection of spinal infection in back pain patients. BMC Musculoskeletal Disorders, 20(1). https://doi.org/10.1186/s12891-019-2949-6
Comments
- {{ error[0] }}