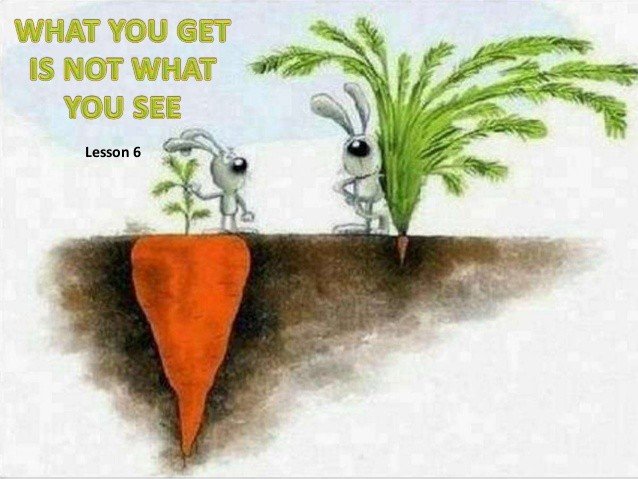
Lumbar structural degeneration, and vertebral spondylolisthesis “WHAT YOU SEE ISN’T ALWAYS WHAT YOU GET, by Rolf Walter”
Case report by Rolf Walter
Lumbar structural degeneration, and vertebral spondylolisthesis
“WHAT YOU SEE ISN’T ALWAYS WHAT YOU GET”
Recently a 77 year old lady in good to excellent general shape came to my praxis complaining of sock like pins and needles distribution on both legs especially during the night or during a small resting break on the couch after lunch. Her general activity level is quite high as compared to her age matches as she practices yoga on a regular base for more than 40 years, likes to walk long distances in the Swiss mountains uphill as well as downhill and she likes to work in her garden. None of the abovementioned activities cause her any trouble.
Interestingly she has no history of backache but her sock-like distribution of pins and needles are present for more than 16 years, which makes her technically, obviously, a chronic patient, just recently slightly increased in intensity! She tends to avoid carrying weights over 10 Kg. because that gives some discomfort in the legs.
Spine movements are pain free in all directions, maybe a bit rigid in extension at the thoraco-lumbar junction, with localized overpressure eliciting local symptoms, otherwise pretty flexible for a lady of her age but not very surprising if you consider her “crush” for yoga which she practices on an almost daily basis.
Neurological examination shows no deficits (not clinically nor on EMG).
As you can see on both X-rays there is impressive degenerative change in the lumbar spine probably in relation to her lumbar scoliosis and to her L3-4 and L4-5 spondylolisthesis. Persons with degenerative changes and even with progressive slippage can be asymptomatic.
There is no available data on dynamic vertebral slippage of the patient but her subjective as well as her physical examination findings do not require, for the time being, any urgent further examination in that direction.
On MRI cystic formation (Tarlov cysts) in the thoracic spine have been documented. There is no available data from medical specialists up to date to give clinical value to the diagnostic presence of thoracic cysts apart from the fact that the patient feels generally well and that there is no neurological dysfunction whatsoever.
“Tarlov cysts, also known as perineural cysts are type II innervated meningeal cysts, cerebrospinal-fluid-filled (CSF) sacs most frequently located in the spinal canal of the S1-to-S5 region of the spinal cord (much less often in the cervical, thoracic or lumbar spine), and can be distinguished from other meningeal cysts by their nerve-fiber-filled walls. Tarlov cysts are defined as cysts formed within the nerve-root sheath at the dorsal root ganglion. Since Tarlov cysts are cysts of the spinal meninges, symptomatic Tarlov cysts by definition cause myelopathy. The etiology of these cysts is not well understood; some current theories explaining this phenomenon have not yet been tested or challenged but include increased pressure in CSF, filling of congenital cysts with one-way valves, inflammation in response to trauma and disease. They are named for neurologist Isadore Tarlov, who described them in 1938”
“Type III cysts” are intra-dural; these are either congenital or caused by trauma; they are rarely associated with other abnormalities and rare in occurrence. About 75% can be found in the dorsal area. Most of the congenital type-III cysts can be found posteriorly to the spinal cord, as opposed to those caused by trauma which can be found anteriorly to the spinal cord”: Source Wikipedia
On visiting her medical dr. she got the prescription of a lumbar semi-rigid corset, probably related to the fact that the medical specialist thinks that the symptoms are being put into relation with the degenerative changes in the back. The patient told the specialist that she did not have the intention to wear the corset, she feels far too good, has no history of lumbar problems and feels her trouble is related to something else than her lower back! The medical dr. insisted that she would take medication (Lirica) which she prefers not to take. When her dr. found out she wasn’t taking her prescribed medication he made a request for a neurosurgical visit where she refuses to go because she feels that this might complicate her situation more than it might actually help!
"Interesting and strong personal view of the patient,apparently she does not feel that bad and is not very influenceable by medical opinions!"
In the end the specialist said that if she doesn’t want to take Lirica and she doesn’t want to see a neurosurgeon than the only option remains physiotherapy!
"Myself and the patient thought it was interesting that physiotherapy came at the very end of therapeutic options!"
It seems that this patient has strong faith in her ability to cope with her current situation which is certainly not always the case in most of my patients.
“A systematic review of quantitative and qualitative research has found strong evidence that patient beliefs about back pain are associated with the beliefs of the clinician with whom they have consulted and moderate evidence that high levels of fear avoidance beliefs in clinicians are associated with high levels of fear avoidance beliefs in their patients. These findings were primarily synthesised from observational research and so were not able to demonstrate causation. However, findings from qualitative interview studies indicate that clinicians influence the beliefs of their patients.”
Ben Darlow; Beliefs about back pain: the confluence of client, clinician and community
Although there seems to be a clear excessive kind of motion around L4 (see video) her main problem seems not to be related to any kind of movement but more to positioning overnight. (Is the thoracic cyst playing a role?) There is some L-R sensation of difference in load transfer from legs to the vertebral column on the cross-trainer (maybe related to her thoracolumbar scoliosis?), but no manifestations of symptoms during this activity. The patient has a radiographic sill sign an increased interspinous gap during flexion to extension motion. Passive physiological intervertebral movements show well palpable increased movements around L3-4 and L4-5 but passive accessory intervertebral movements elicit no symptoms whatsoever.
We agreed upon that the first step should be if in some way we can change positioning over night to make her more comfortable with less symptoms! From there we go step by step and see if there may be some improvement achievable.
After 4 treatments in about 4 weeks;
Positioning her thoraco-lumbar junction in side lying position with a cushion seemed to calm down some of the intensity of the symptoms at first and treating her thorax with passive and active movements increasing her thorax dynamics has brought a sensitive reduction in her symptoms, the sock like distribution is gone when she is taking her after lunch nap on the couch and reduced overnight (some nights have been without symptoms, some with only partial symptoms like only in the lower part of the shin and not under the foot or only and the foot dorsum a line like electrical kind of symptom without the pins and needles.) We both feel that we are on an interesting therapeutic path for the moment, I stressed the fact that she should keep up her regular activity level and feel free to do whatever she feels is good for her back, she seems very much “tuned-in” with her body and that is always a great help.
We are in agreement on an active approach which fits the character as well as the individual demands of the patient.
The clinical value of her X-rays and MRI has been discussed and put into context
What you see on the X rays and partially on clinical examination (suspect of lumbar structural instability) isn't necessarily related to what the patient suffers! There are no data available on structural lack of stability, there are no clinical signs of instability behavior. The patient has no history of back pain and leads an active and healthy lifestyle. For the time being the first indicators after initial treatment are positive, we have to monitor how she is going to react in the next weeks to months. There seems to be no immediate need for further medical examination procedures.
Brinjikji W., et al; Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations, AJNR Am J Neuroradiol. 2015 April ; 36(4): 811–816
Kang A. et al, New physical examination tests for lumbar spondylolisthesis and instability:low midline sill sign and interspinous gap change during lumbar flexion-extension motion , BMC Musculoskeletal Disorders (2015) 16:97
Geerse W.K., Bilateral leg symptoms e The T10 syndrome? A case report, Manual Therapy 17 (2012) 251-254
Darlow B., Beliefs about back pain: the confluence of client, clinician and community, International Journal of Osteopathic Medicine, 2016








Comments