Lateral elbow pain? a need for dualistic reasoning!
Lateral elbow pain; finding the pain driver? A need for dualistic reasoning!
Lateral elbow pain and movement dysfunction has been subject to a great amount of studies with a wide variability of produced results (5,9). A vast number of local structures and local biomechanics have been accused of being the potential peripheral, structural, driver of symptoms, either through ultrasonographic differentiation (17) or through other means of instrumental investigations (17, 18, 19, 20):
-Altered joint surfaces (angiofibroblastic and hyaline degeneration, inflammation and synovial hypertrophy, fractures, altered joint boundaries)
-Degeneration of the lateral elbow recess
-calcifications, neovascularities
-Lateral synovial fold impingement
-Altered osteo- and arthrokinematics (f.e: posterolateral instability)
-Joint capsule and ligaments
-Muscles and tendons (tear, intra- and peritendineous alterations)
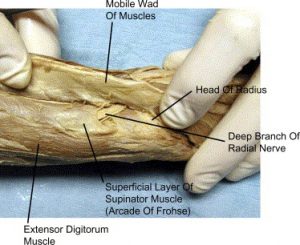
-Radial, ulnar and the median nerves compression (note the deep branch of the radial nerve just distally of the radial head)
-Several layers of innervated connective tissue
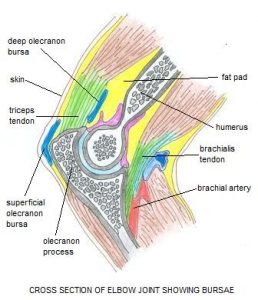
-bursae
Besides local structures more remote areas and remote structures have been mentioned to be involved in referred or irradiated pain into the elbow as well as comorbid pain areas and may influence the rehabilitation approach (21).
One of the first and probably main difficulties in trying to identify neuro-musculoskeletal drivers of lateral elbow pain is the fact that central sensitization is suggested to be involved in lateral elbow pain (1,5,6,7,8,9,11,13,14,17). Anatomical representations of single anatomical structures in the central nervous system are poorly represented if at all (4). Functional and coordinated components of position and motion are not the muscles and joints, but movements and performed actions (4) and motor units are more represented by behavioral tasks rather than by motor nuclei (2,3). A number of patients identified as having clinical profile for lateral elbow pain with structural alterations also exhibited evidence of altered pain modulation and therefore a profile which suggests poor prognostic indicators (5,9). This requires alertness for reasoning in two directions; peripheral or structural reasoning if the clinical picture forces us to reason at musculoskeletal level (history of recent trauma or overuse) but at the same time raised awareness of possible contemporary central modulation which takes us away from searching a peripheral driver).
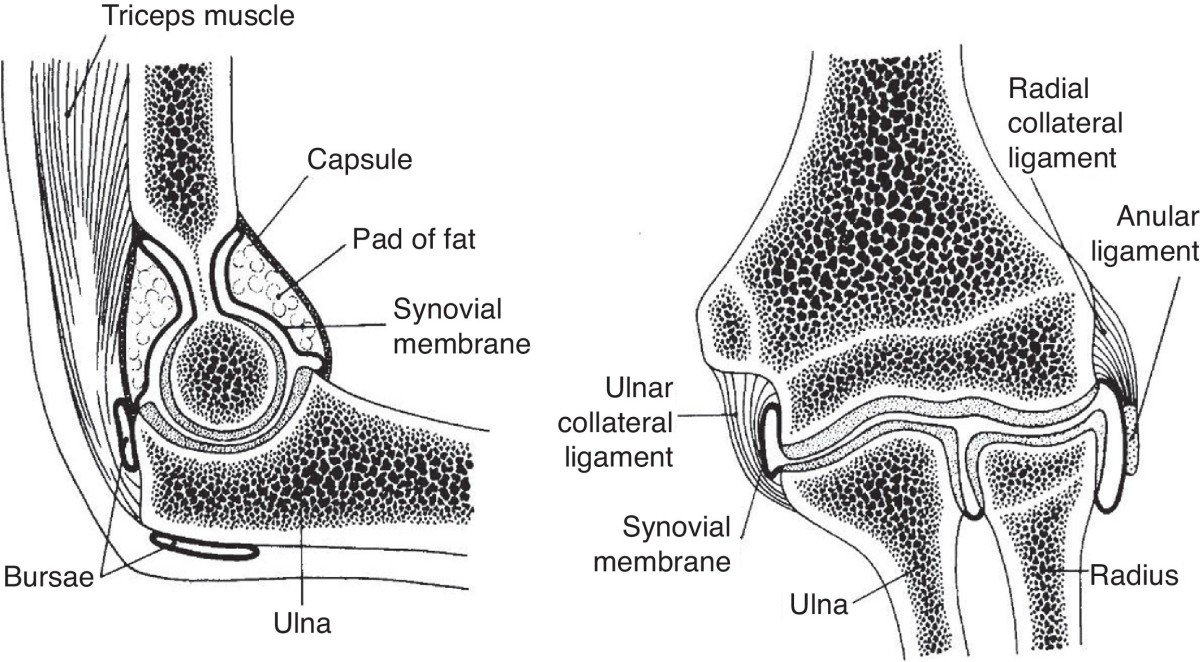
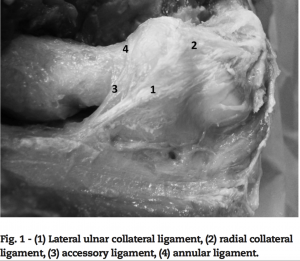
Structural reasoning and clinical differentiation, when the pain is localized at the elbow, may be inviting. Limitations for structural differentiation are though, without doubt, anatomical blending of tissues at the lateral elbow compartment at the lateral ligament complex; the radial collateral ligament, the lateral ulnar collateral ligament, and the annular ligament.
“The lateral ulnar collateral ligament also arises from the lateral epicondyle, and its fibers may be indistinguishable from those of the radial collateral ligament. It then courses posteriorly as it cradles the radial head and coalesces with annular ligament fibers as it inserts on the supinator crest of the ulna (10). Although the entire lateral collateral ligamentous complex works in conjunction to provide resistance against varus stress and posterolateral rotary instability, isolated lateral ulnar collateral ligament injuries may lead to posterolateral instability (isolated radio-capitellar subluxation) with an intact annular ligament stabilizing the radioulnar joint (10)”.
Anatomical ligamentous blending and conjunct involvement of the lateral ligamentous complex makes structural differentiation based on clinical examination therefore extremely challenging.
Several myofascial structures are thought to blend with the lateral ligamentous complex and are described by the dutch anatomist Jaap van der Wal; “Most of the collagenous fibers in the proximal lateral cubital region appear to be interposed between skeletal tissue and muscle fascicles, therefore no separate entity such as a collateral radial ligament could be demonstrated”. The same situation appears to be true for the annular radial ligament, in fact, the so-called annular ligament does not exist; it is an integrated part of the aponeurotic layer of connective tissue via which supinator muscle fibers insert to the lateral epicondyle (4).”
The anatomical observations made by Van der Wal using a connective tissue “sparing” type of dissection allows us to have a different look on previously described anatomy and highlights anatomical interconnections between several myofascial layers and so-called ligaments, this seems to shed a different light on presumed clinical capacity of differentiating singular tissue’s using a movement at the elbow.
The above picture is from the article of Jaap Van der Wal, 2009 and shows convergence of connective tissue surrounding muscles at the lateral epicondyle of the elbow.
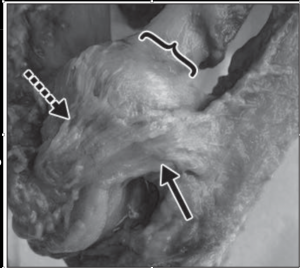
The pictures below show the blending of ligaments around the elbow complex. Variations of ligamentous architectural orientation have been previously described in literature (10). As well as several anatomic variations in bony and ligamentous structures around the elbow. The dotted arrow indicates the radial collateral ligament and the solid arrow indicates the lateral ulnar collateral ligament, the bracket indicates the annular ligament. (note the blending of all three ligaments)
Connective tissue and fasciae are richly innervated, fascial layers may thus play an important role in proprioception and nociception (4). This makes structural differentiation based on clinical examination very challenging.
In summary, several important reasons may make structural differentiation in clinical examination challenging:
- Central sensitization is a potential mechanism behind lateral elbow pain. This makes the search for a distinct peripheral driver foremost obsolete.
- Peripheral structures are poorly represented in the central nervous system. Central representations are more linked to behavioral tasks.
- In case of a peripheral driver, anatomical blending at the elbow of a great variety of tissues with consequent multi-structural involvement during loading makes clinical selection of single structures extremely difficult if not impossible.
- Most symptom provocations, even if reliable and consistent, are not necessarily pathognomonic for any particular anatomical tissue.
- As previously reported in one of my blogs on structural differentiation, mechanical loading and symptom provocation is not an infallible indication of location of the pathological source and structural interpretation should be undertaken with great care, not only at the elbow
- Rehabilitation should be based on extensive examination of potential biological as well as psychosocial contributors to lateral elbow pain. Hypothetical -deductive reasoning and careful, individual and goal orientated, planning of rehabilitation in concordance with the patient is mandatory.
- 1. Jespersen A. et al, Assessment of pressure-pain thresholds and central sensitization of pain in lateral epicondylalgia, Pain Med.2013 Feb;14(2):297-304
- 2. Loeb GE. Task groups—a proposed functional unit for motor control. Abstr Soc Neurosci. 1982;8:272–277.
- 3. Loeb GE. Motoneurone task groups: coping with kinematic heterogeneity. J Exp Biol. 1985;115:137–146.
- 4. Van der Wal J., Connective tissue architecture and proprioception, international journal of therapeutic massage and bodywork, Vol. 2, No 4, Dec 2009
- 5. Bisset L. et al, Characterising pain and modulation mechanisms underpinning lateral elbow tendinopathy: a case control study. Manual Therapy 25 (2016)
- 6. Fernandez-Carnero J. et al, Widespread mechanical pain hypersensitivity as sign of central sensitization in unilateral epicondylalgia: a blinded, controlled study. Clin J Pain.2009 Sep;25(7):555-61
- 7. Woolf C. Central sensitization: Implications for the diagnosis and treatment of painPain. 2011 Mar; 152(3 Suppl): S2–15.
- 8. Arendt-Nielsen L.et al., Basic aspects of musculoskeletal pain: from acute to chronic pain, J Man Manip Ther. 2011 Nov; 19(4): 186–193.
- 9. Bisset L.M. et al, Physiotherapy management of lateral epicondylalgia, Journal of Physiotherapy 61: 174–181]
- 10. Tomsick S.D. et al, Seminars in Musculoskeletal Radiology 14(4):379-93 · September 2010
- 11. Nijs J. et al Thinking beyond muscles and joints: Therapists’ and patients’ attitudes and beliefs regarding chronic musculoskeletal pain are key to applying effective treatment, Manual Therapy 18 (2013) 96e102
- 12. A critical look at Structural differentiation. Rolf Walter, IMTA Blog
- 13. Palpation, passive movement exploration, can you feel it? Rolf Walter, IMTA blog
- 14. Plinsinga M. et al, Evidence of nervous system sensitization in commonly presenting and persistent painful tendinopathies: a systematic review, JOSPT, 2015
- 15. Obuchowicz R., Ultrasonographic Differentiation of Lateral Elbow Pain, Ultrasound International Open 2016; 2: E38–E46
- 16. Hengeveld E., Banks K., Maitland’s periphereal manipulation, 5th edition
- 17. Obuchowicz R, Bonczar M. Ultrasonographic Differentiation of Lateral Elbow Pain, Ultrasound International Open 2016; 2: E38–E46 18. Grayson D.E. et al, The Elbow: Radiographic Imaging Pearls and Pitfalls, seminars in radiology 2005
- 18. Obradov M. et al, ultrasonographic findings for chronic lateral epicondylitis, JBR–BTR, 2012, 95 (2)
- 19. De Zordo T. et al, Real-Time Sonoelastography of Lateral Epicondylitis: Comparison of Findings Between Patients and Healthy Volunteers, AJR: 193, July 2009
- 20. Coombes B.K. et al, Management of Lateral Elbow Tendinopathy, One Size Does Not Fit All , JOSPT, vol 45, no 11, 2015
- 21. Cook C.E., Hegedus E.J., Orthopedic physical examination tests, second edition.





Comments