Clinical Reasoning during direct access
Hey you.
Yes YOU!
I have some difficulties with my lower back and hopefully you can give me some thoughts and some tips how to handle it.
I am 45 years old, 1.72 meters tall and my bodyweight is about 72 kg. I am working as a quality control manager for a pharmaceutical lab, means I am sitting like half of the day and sometimes lifting boxes of 4.5 to 9 kg.
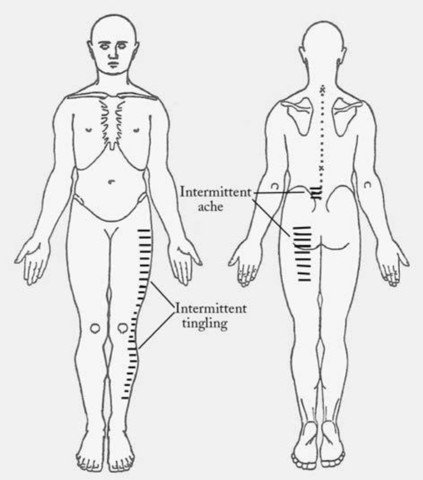
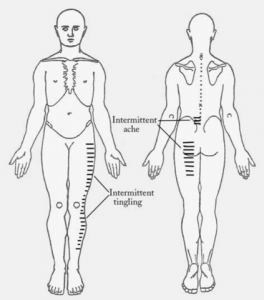
I have already drawn a picture of my symptoms for you. The pain starts in my lower back on the left side and extends to my posterior thigh. This pain is not constantly there, it depends on what I’m doing. It’s the same for the tingling on the lateral frontside of my leg. Sometimes it’s more and sometimes it’s less. But this depends also on what I am doing and comes and goes parallel with the pain in the back and leg.
Hey there, I am your inner clinical reasoning voice. I just received some information and we need to talk about them. Do you think the patient’s problem is more mechanical or non-mechanical? How many sources for the symptoms do you expect? Are there any precautions we have to be careful of?
Activities that increase my symptoms are lying supine, coughing and sneezing, prolonged walking and sitting for longer than an hour. Using a heat pad for the lower back and taking 200 mg Ibuprofen like every 4 hours makes me feel better.
I feel not much pain in the morning, it gets more intense in the evening or when I try to fall asleep. I also wake-up sometimes because of the pain but when I find a comfortable position I can quickly fall asleep again.
I already have those symptoms for a couple of months but I cannot remember any incident that explains the onset of them. Just the tingling started like a week ago. I already had some lower back pain in the past but it never limited me and I never had symptoms in the thigh.
Besides the Ibuprofen I don’t take any other drugs. I don’t have hypertensions, diabetes, previous cancer history or weight loss, bladder and bowl function is normal and I have no other concerns pertaining to general health. I don’t smoke and I haven’t taken steroids or anti-coagulation drugs in the past. You are the first person I am talking to about my issue, so I have no recordings of previous examinations.
Hey me again. Let’s think about this. What about your previous thoughts (mechanical/non-mechanical, sources, precautions)? Did they change?
Are the symptoms related to a certain movement direction? Which area would you investigate further? What would you expect to find during a physical examination?
Do you recognize a clinical pattern?
This are the results of my first physical examination (summary):
Gait slightly antalgic (trying to avoid pain) while weight bearing on the left lower extremity.
Active Movements
- Extension moderate decreased, reproduction of lower back pain *
- Flexion unsuspicious
- LatFlex left slightly decreased, reproduction of lower back and thigh pain *
- LatFlex right unsuspicious
Neurological exam revealed muscle weakness of the left hip flexors and knee extensors. Achilles- and patellatendon reflexes were bilaterally ok.
Passive Movements
- Hip Flex, internal and external rotation was bilaterally similar, with no change in symptoms
- Hip adduction in 90° flexion - 20° less compared to right side, reproduced posterior thigh symptoms *
- Straight leg raise right side 60°, tightness in hamstring muscles
- Straight leg raise left side 45°, increased left posterior thigh pain *
Do the findings match your previous thoughts? What else would you have examined?
This was my treatment:
1st Session:
- Assessment as described above
- Treatment:
- General lumbar rotational oscillatory technique in side lying on the right side for 5 minutes (reassessment unchanged)
- Homework: similar to the treatment technique as automobilisation every 2 to 3 hours
- Education in appropriate sleeping and sitting postures
2nd Session (1 week later)
- Overall unchanged
- Slight temporary pain reduction after the exercise
- Reassessment unchanged
- Additional Assessment:
- Central PA C5 reduced mobility (compared to other spinal levels), reproduction of back pain, posterior thigh pain and anterolateral tingling *
- Hip Ext right 15°, no symptoms
- Hip Ext left 10°, reproduction of back pain, posterior thigh pain and anterolateral tingling *
- Reduced strength of left hip abductors *
- Negative prone knee bend test bilaterally
- Treatment:
- Like in the 1st Session
- Hip stretching to address the findings there
Further sessions:
- Treatment was once a week and consisted of the interventions mentioned in “2nd session”
- Overall symptoms got worse
- Sitting tolerance decreased
- Symptoms became more constant
- Gait became more antalgic, patient had to use a single-point cane
- Reassessment didn’t change
Since the first session, 29 days have passed. Instead of improving, the patient’s symptoms got worse. Why could that be? Does this fit to our further hypothesis? What should we change to improve the patient’s condition?
Hey all of you, now this time its Sebastian from the IMTA ;)
The patient that is described above is a case report that has been published in JOSPT in 2005 (Ross and Bayer, 2005). I think this can be a typical patient in your clinic: low back pain with some radiating symptoms (in this case pain and tingling). It can be provoked and relieved with certain movements and prolonged positions. There have been some points in the physical examination that haven’t been fully clear to me like:
- lumbar rotation wasn’t mentioned
- what did they mean with weakness in the neurological exam? (“normal” muscle weakness or reduced rebound?)
- no sensitizing movement during the straight leg raise, so no clear information about a potential nociceptive source
But overall, the findings display a quite mechanical nociceptive issue (presumably from the lower lumbar spine) with additional neurogenic input.
Even the night pain reacts quite mechanical as it got relieved by turning over and about 58 % of patients with low back pain wake up at night without displaying an underlying serious pathology (Premkumar et al., 2018).
However, after 4 weeks of intervention we have to re-evaluate our findings:
- Night pain
- Aggravating pain (need for a cane to walk) for no obvious reason
- Aggravating neurologic symptoms
- Not responding to therapy
To shorten it up a little bit: the patient was finally diagnosed with a small cell carcinoma of the lung with multiple areas of bony metastases (in the spine, sacrum and left pelvis/hip).
I discussed this case with some friends that work in direct access scenarios as physical therapists. They confirmed that sometimes time, reassessment and ongoing clinical reasoning are the most important tools to identify some serious pathologic mechanisms.
I also had some take away’s after reading this case again:
- Symptom reproduction (active and passive) and short-term relief do not rule out serious pathology (see also case report by Mabry et al., 2014)
- Pain relief by turning in bed isn’t either
- Do your re-assessments
- Every one of us performs direct access (a friend or family member asking for advice, a patient has some change in symptoms during waiting for his first appointment, patient referred with neck pain for example asks you for advice for his lower back)
So now you shouldn’t panic and send every patient back to the physician ;) The most important question during our clinical reasoning process should be: do the features (still) fit?
Thanks for reading,
Sebastian
#directaccess #redflag #reflagscreening #lowbackpain #specificpain #maitland #imta #sebsebsen #löscher
Mabry, L.M., Ross, M.D., Tonarelli, J.M., 2014. Metastatic cancer mimicking mechanical low back pain: a case report. J. Man. Manip. Ther. 22, 162–169. https://doi.org/10.1179/2042618613Y.0000000056
Premkumar, A., Godfrey, W., Gottschalk, M.B., Boden, S.D., 2018. Red Flags for Low Back Pain Are Not Always Really Red: A Prospective Evaluation of the Clinical Utility of Commonly Used Screening Questions for Low Back Pain. J. Bone Jt. Surg. 100, 368–374. https://doi.org/10.2106/JBJS.17.00134
Ross, M.D., Bayer, E., 2005. Cancer as a Cause of Low Back Pain in a Patient Seen in a Direct Access Physical Therapy Setting. J Orthop Sports Phys Ther 35, 9.





Comments