The cause of the cause…looking for our blind spots in knowledge and understanding of clinical patterns
Experienced clinicians use pattern recognition in their clinical reasoning based on an extensive knowledge base to search for familiar patterns (Feltovich & Barrows, 1984). Pattern recognition offers a quick and effective way to come to a hypothesis as a base to start patient management. However management based on pattern recognition only, may lead to clinicians following their favourite hypothesis and trying to ‘making the features fit’ within the framework of this hypothesis (Maitland et al, 2005). In order to control for this bias, a more robust process of hypothetico-deductive reasoning, in which multiple hypothesis are tested, is recommended. The latter depends on the ability of clinicians to interpret subjective and physical findings and will highly depend on their knowledge base (Ryder, 2018). By listening and thus adopting narrative reasoning skills, the clinician tries to understand the story of the patient (Edwards et al, 2006) and integrates the patient’s thoughts and beliefs (Cooper et al 2008). Information given by the patient must be recognised as relevant and interpreted by the therapist. This process depends strongly on the therapist’s knowledge base. Sound clinical reasoning requires metacognition and critical reflection, which are both important to recognise limitations in knowledge (Jones, 2013). If the clinician thinks information is lacking, clarification for completeness can be obtained by the use of ‘screening questions’ for other types of symptoms.
IMTA courses advocate the conscious use of Clinical Reasoning starting right from the first moment the patient consults us following through physical examination, treatment & overall management until the very last encounter. Reassessment and reflection are key in this process and are especially important when “features don’t fit” and hypotheses have to be adjusted. Some patients present with conditions that seem to fit in a straight forward pattern, but in the end, in order to really promote recovery and solve the patient’s problem, both clinician and patient have to investigate, examine and reflect further to find of the cause of the patient’s problem. Especially in areas where most Musculoskeletal Physiotherapists (MSK PT) might have blind spots in knowledge and understanding of underlying mechanisms and connections.
Blind spot: pelvic floor
Some patients made me aware of my blind spot and the necessity to expand my knowledge and skills to recognise the cause of the cause of persistent symptoms around the pelvis. I’d like to share some of their stories.
Patient example 1:
A young mother and IT specialist, presented with the diagnosis: “Proximal Hamstring Tendinopathy”. Her main problem: buttock pain while working sitting at her desk.
The patient came to see us after almost a year of failed PT treatment addressing the tendon locally and applying black-roll and stretches herself. It turned out that she also suffered from incontinence when jogging since the birth of her second child 3 years ago. She loved to go for a run and she started right after delivery to get back in shape. She was highly frustrated that, no matter how hard she tried (Pilates core exercises every day & Cross-fit group 3x a week), she was not able to get back to her old level of condition. Only after referral to a pelvic health specialist, she was soon be able to run without problems. Gradually recovering muscle balance (including relaxing her core), she is now symptom free in sitting as well.
![]() What does the literature say? CrossFit exercises, which involve jumps were often found to be related to urinary incontinence. Possibly elevated intra-abdominal pressure and reaction forces on the pelvic organs could be involved in these high-impact activities. Athletes are recommended to integrate strengthening the pelvic floor in their training programme. Trainers should carefully select exercises to avoid overload (Dominguez-Antuna et al, 2022).
What does the literature say? CrossFit exercises, which involve jumps were often found to be related to urinary incontinence. Possibly elevated intra-abdominal pressure and reaction forces on the pelvic organs could be involved in these high-impact activities. Athletes are recommended to integrate strengthening the pelvic floor in their training programme. Trainers should carefully select exercises to avoid overload (Dominguez-Antuna et al, 2022).
Patient example 2:
A male patient with pelvic girdle pain and parästhesia due to excessive  cycling, developped a neuropathy of the superficial branches of the pudendal nerve. Because the patient also suffered sexual dysfunction he was referred to a Pelvic Health PT.
cycling, developped a neuropathy of the superficial branches of the pudendal nerve. Because the patient also suffered sexual dysfunction he was referred to a Pelvic Health PT.
![]() What does the literature say? In a review on the topic, Chiaramonte et al (2021), found that both beginners and experienced cyclists can develop pudendal nerve problems. Bicycle design, posture as well as seat design seem to play a role. Standing on pedals, rest and shifting to a higher gear were recommended as management. Furthermore, pudendal neuropathy is described as an “underrecognized cause of pelvic pain that can be difficult to diagnose and treat” although often associated with cycling also doing squat-based exercises can be involved as a cause (Kasitinon et al, 2021).
What does the literature say? In a review on the topic, Chiaramonte et al (2021), found that both beginners and experienced cyclists can develop pudendal nerve problems. Bicycle design, posture as well as seat design seem to play a role. Standing on pedals, rest and shifting to a higher gear were recommended as management. Furthermore, pudendal neuropathy is described as an “underrecognized cause of pelvic pain that can be difficult to diagnose and treat” although often associated with cycling also doing squat-based exercises can be involved as a cause (Kasitinon et al, 2021).
Patient example 3:
An elderly obese patient with low back pain, pelvic girdle pain and left hip pain, who also had pelvic floor dysfunction and diverticulitis as comorbidities. This patient had incontinence problems ever since she had her first child 50 years ago! She told me that she thought it was normal to have these kind of problems after delivery…
Pelvic floor and lumbopelvic pain
Recent literature is showing that there is a close correlation between dysfunction of the pelvic floor and lumbopelvic pain. The pelvic floor complex is involved in many functions apart from its biomechanical role in pelvic girdle stability, control, and force transfer (Pool-Goudzwaard, 2020). Pelvic floor dysfunction is sometimes called “a silent epidemic,” which is “under-recognized and insufficiently managed” (Frawley, 2019).
Pelvic floor dysfunction 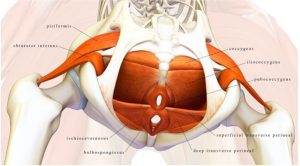 is an umbrella term for any abnormality or impairment within the pelvic floor and the systems which are involved. This includes the pelvic floor muscles, pelvic organs, urogenital and colorectal systems. Pain in the pelvic floor region can also arise from visceral pathology and there are serious pathologies that occur in the pelvic region that may be missed.
is an umbrella term for any abnormality or impairment within the pelvic floor and the systems which are involved. This includes the pelvic floor muscles, pelvic organs, urogenital and colorectal systems. Pain in the pelvic floor region can also arise from visceral pathology and there are serious pathologies that occur in the pelvic region that may be missed.
Disregarding the pelvic floor as an important part of pelvic girdle pain may result in inappropriate management of a patient and may cause unnecessary delay in the patient’s condition getting better (Röscher, 2021). Quite often, patients presenting with lumbopelvic, or pelvic girdle pain have associated pelvic floor muscle dysfunction. In a study by Dufour et al (2018), in a cohort of 85 females with lumbopelvic pain 95.3% had a degree of pelvic dysfunction.
Musculoskeletal (MSK) Physiotherapists ideally have a basic understanding of the pelvic floor and its associated dysfunctions so that they will be able to screen these patients, and if indicated, refer them on to a pelvic floor health professional (De Ruijter & Röscher, in press).
Roles and boundaries of the competencies of a MSK therapist in relation to the pelvic floor
During the C/O every MSK therapist should be prepared to include specific questions on possible pelvic floor dysfunction as the cause of the cause of as a contributing factor to the patient’s symptoms. Typically, patients will not automatically share information on pelvic floor dysfunction in a Musculoskeletal setting. Therefore, it can be difficult for the therapist to ask specific questions regarding pelvic floor dysfunction. Perhaps the MSK therapist feels embarrassed or perceives that the patient might feel embarrassed by these type of questions. Even in a medical setting, Ben Charif et al (2016), found that only 20% of cancer patients told their doctors about sexual dysfunction. In order to facilitate this situation supplying a questionnaire to the patient might be a way to obtain information in a non-threatening way. In case the questionnaire indicates involvement of the pelvic floor, it will be easier for the therapist to use this information and use it to bridge for further clarification.
Based upon the Australian Pelvic Floor Questionnaire and Frawley et al (2021), Röscher (2022) suggests to use the following question to gain consent for asking pelvic floor related questions: “Some people with pelvic pain also experience problems with their pelvic floor. Would it be okay, if I asked you questions about your bladder, bowel and sexual function?”
- To specifically ask for bladder dysfunction, you could ask: “Do you leak urine with coughing, sneezing, laughing or exercising?” “Does urine leak when you rush or hurry to the toilet or you can’t make it in time?”
- Questions to ask about bowel dysfunction: “Do you feel constipated or struggle to empty your bowels?” “Do you ever leak stool?”
- Finally, to ask about pelvic floor muscle motor symptoms: “Does your pelvic floor feel loose, lax, gaping, sagging, open, weak, bulging, heavy, full, or difficult to relax, tight, tense, narrow, or constricted?” (Röscher, 2021).
In case the MSK PT has a hypothesis that the pelvic floor might possibly be involved in the patient’s main problem, referral to a pelvic health specialist is needed. The task of the pelvic health specialist involves specific ultrasound assessment, and external observation and internal vaginal or rectal examination. Pelvic Floor Dysfunctions can be divided in various specific disorders and the management might vary accordingly (Frawley et al, 2021).
Without specific training and experience with assessment and treatment of Pelvic Floor Dysfunctions, just starting some kind of pelvic exercises with these patients should be discouraged as it could worsen the patient’s condition. It is highly recommended to start building a network of skilled colleagues with experience in this field, collaborate and expand your professional horizon by asking the appropriate questions in trying to discover the “cause of the cause” of the patient’s signs and symptoms.
References:
Ben Charif, A., Bouhnik, A-D., Courbière, B., Rey, D., Préau, M., Bendiane, M-K., Peretti-Watel P., and Mancini, J. (2016). Sexual Health Problems in French Cancer Survivors 2 Years after Diagnosis—the National VICAN Survey. Journal of Cancer Survivorship 10, no. 3 (June 2016): 600–609. https://doi.org/10.1007/s11764-015-0506-3.
Chiaramonte, R., Pavone, P., and Vecchio, M. (2021). Diagnosis, Rehabilitation and Preventive Strategies for Pudendal Neuropathy in Cyclists, A Systematic Review. Journal of Functional Morphology and Kinesiology 6, no. 2: 42. https://doi.org/10.3390/jfmk6020042.
Cooper et al (2008) in: Petty, N. J., & Ryder, D. (Eds.). (2017). Musculoskeletal Examination and Assessment E-Book: A Handbook for Therapists. Elsevier Health Sciences.
De Ruijter, R., Röscher, M. in: Hengeveld, E. & Bucher-Dollenz, G. (in Press). The Maitland Concept of NMSK Physiotherapy - Assessment and Management of NMSK Movement Functions. Vol 2: Clinical Application. 6th ed. Chapter: Pelvic Girdle, examination and management. Elsevier, Oxford.
Dominguez-Antuña, E., Diz, J. C., Suárez-Iglesias, D. and Ayán C. (2022). Prevalence of Urinary Incontinence in Female CrossFit Athletes: A Systematic Review with Meta-Analysis. International Urogynecology Journal, May 30. https://doi.org/10.1007/s00192-022-05244-z.
Dufour, S. (2018). Association between Lumbopelvic Pain and Pelvic Floor Dysfunction in Women_ A Cross Sectional Study. Musculoskeletal Science and Practice, 7.
Edwards, I., Jones, M., and Hillier, S. (2006). The Interpretation of Experience and Its Relationship to Body Movement: A Clinical Reasoning Perspective. Manual Therapy 11, no. 1: 2–10. https://doi.org/10.1016/j.math.2005.10.002.
Feltowich, P.J. and Barrows, H.S., (1984). Issues of generality in medical problems solving. In: Petty, N. J., & Ryder, D. (Eds.). (2017). Musculoskeletal Examination and Assessment E-Book: A Handbook for Therapists. Elsevier Health Sciences.
Frawley, H. C., Neumann P., and Delany, C. (2019). An Argument for Competency-Based Training in Pelvic Floor Physiotherapy Practice. Physiotherapy Theory and Practice 35, no. 12: 1117–30. https://doi.org/10.1080/09593985.2018.1470706.
Frawley, H., Shelly, B., Morin, M., Bernard M., Bø, K., Digesu, G.A., Dickinson, T. An International Continence Society (ICS) Report on the Terminology for Pelvic Floor Muscle Assessment. Neurourology and Urodynamics 40, no. 5 (June 2021): 1217–60. https://doi.org/10.1002/nau.24658.
Hengeveld, E. & Banks, K. (Eds.). (2013). Maitland's Vertebral Manipulation: Management of Neuromusculoskeletal Disorders-Volume 1 (Vol. 1). Elsevier Health Sciences.
Jones, M. in: Hengeveld, E. & Banks, K. (Eds.). (2013). Maitland's Vertebral Manipulation: Management of Neuromusculoskeletal Disorders-Volume 1 (Vol. 1). Elsevier Health Sciences.
Kasitinon, D., Kelly, B., Price, T. L., Chhabra, A., & Scott, K. M. (2021). Pudendal nerve injuries in sports and exercise: a case series of pudendal neuropathies from squats. Journal of Women's Health Physical Therapy, 45(1), 3-9.
Maitland, G. D., Hengeveld, E., Banks, K., & English, K. (2005). Maitland's vertebral manipulation: Elsevier Butterworth.
Pool-Goudzwaard, A., Beales, D. and Bussey, M. (2020). Introduction to the Special Issue on Pelvic Pain. Musculoskeletal Science and Practice.48 102168. https://doi.org/10.1016/j.msksp.2020.102168.
Röscher M. (2021). Course Slides from “The Functional Pelvis” (online course). www.physioskills.com.au
Ryder D. In: Petty, N. J., & Ryder, D. (Eds.). (2017). Musculoskeletal Examination and Assessment E-Book: A Handbook for Therapists. Elsevier Health Sciences.






Comments