20 years of pain education – what can we learn from the literature?
Why is pain education important?
Pain education is a biopsychosocial approach that aims to decrease the threat value of pain by reconceptualizing pain and improving patients’ knowledge about pain. Broadly, pain education can be divided into two components: pain science education and education about pain management. Pain education can give hope and answers two important questions of patients: “Why do I hurt?” and "What can I do about my pain?".
Pain education in the literature
Pain education, also known as „explain pain“ (Butler and Moseley 2003, Moseley and Butler 2017) and „pain neuroscience education“ (PNE) (Nijs et al. 2011, Louw et al. 2011) has been studied for the last 20 years. Research on the assessment and discussions about pain education have increased greatly in recent years. Entering the search term “pain neuroscience education” in PubMed leads to 9 research articles published in 2002 and 444 articles in 2021. This steep increase in articles on the topic of pain education shows the great interest in this topic.
Integration of pain education into clinical practice
Pain education is well established in health care, but many questions remain unanswered. The guidelines for chronic musculoskeletal (MSK) pain conditions mention pain education as an important treatment method, but its application in practice often still lags behind (Lin et al. 2020). Changing patients' beliefs about their pain requires patient willingness, consistent messages, recurrent interactions and coaching to achieve sustainable change. Pain education is important for the clinical implementation of the biopsychosocial treatment approach and forms the basis of interdisciplinary pain management (Beetsma et al. 2021, Eneber-Boldon et al. 2020).
Studies on pain education
Initially, pain education was mainly studied as a single treatment method for patients with chronic low back pain (Moseley 2002). Over the years, clinical experience and study results have shown that pain education cannot be used in isolation. Today, pain education is predominantly studied in combination with other treatment modalities for different pain conditions and populations, including postoperative pain, acute and chronic pain conditions, different age groups and socioeconomic conditions (Andias et al 2018, Orhan et al. 2019, Saracoglu et al 2020, Traeger et al. 2019). Qualitative studies examining patients' views and needs in relation to pain education have provided additional valuable information (Leake et al. 2019)
What have we learned from the existing literature?
- Pain education is most effective when combined with other treatment modalities
- Pain education should be tailored to the individual needs of the patient
- The patient should be able to make sense of their pain
- Thorough assessment, good communication skills and a therapeutic alliance are the basics
- Pain education requires active engagement of the patient
(Jones et al. 2020, King et al 2018, Nijs et al. 2020, Robins et al. 2016, Eneberg-Boldon et al. 2020)
How should we implement patient-centred needs?
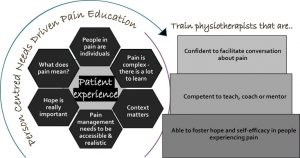
Quantitative studies assessing the patient's perspective can provide evidence on how to tailor pain education to the patient. Tompson et al. (2022) conducted a qualitative systematic review and developed a model to better tailor pain education to individual patient needs (Fig. 1).
Fig. 1 A patient-centred approach to pain education (Thomson et al. 2022).
In addition, Thompson et al. (2022) highlighted the following important considerations for individualised pain education:
- The focus of pain education should be on the impact of pain
- Listen to and believe patients' stories
- Health professionals should reflect on their own attitudes to pain and how this might impact on their clinical practice
Take-home message
Pain education is part of daily evidence-based clinical practice. Critically evaluating our own pain concepts and the values of our patients will help us to develop further. It is necessary to stay up to date in modern pain education.
Stay tuned and keep learning.
Yours sincerely
Gerti Bucher-Dollenz
IMTA Senior Teacher
Literature
Andias R., Neto M. and Siva A.G. (2018) The effects of pain neuroscience education and exercise on pain, muscle endurance, catastrophizing and anxiety in adolescents with chronic idiopathic neck pain: a school-based pilot, randomized and controlled study. Physiother Theory Pract 34(9):682-691. https:// doi.org/10.1080/09593985.2018.1423590
Beetsma A.J., Reezingt R.R. and Reneman M.F. (2021) Knowledge and attitudes toward musculoskeletal pain neuroscience of manual therapy postgraduate students in the Netherlands. Musculoskeletal Science and Practice 52:102350. https://doi.org/10.1016/j.msksp.2021.102350
Eneberg-Boldon K., Schaack B. and Joyce K. (2020) Pain neuroscience education as the foundation of interdisciplinary pain treatment. Phys Med Rehabil Clin N Am. 31 (4): 541-551.https://doi.org/10.1016/j.pmr.2020.07.004
Jones C.K., Tocco E.C., Mashall A.N., Valovic McLeod T.C. and Welch Bacon C.E.(2020) Pain education with therapeutic exercise in chronic nonspecific low back pain rehabilitation: a critically appraised topic. J Sport Rehabil 29(8):1204-1209. https://doi.org/10.1123/jsr.2019-0345
King R., Robinson V., Elliott-Button H.L., Watson J.A., Ryan C.G., Martin D.J. (2018) Pain reconceptualization after pain neurophysiology education in adults with Chronic Low Back Pain: A qualitative study. Pain Res Manag Sept 12. https://doi.org/10.1155/2018/3745651
Leake H.B., Moseley G.L., Stanton T.R., O’Hagan E.T. and Heathcote L.C. (2021) What do patients value learning about pain? A mixed-methods survey on the relevance of target concepts after pain science education. Pain 162(10): 2558-2568. https://doi.org/10.1097/j.pain.0000000000002244
Lin I, Wiles L, Waller R, Goucke R, Nagree Y, Gibberd M, Straker L, Maher C, O’Sulliva P. (2020) What does best practice care for musculoskeletal pain look like? Eleven consistent recommendations from high-quality clinical practice guidelines: systematic review. Br J Sports Med.54:79–86. https://doi.org/10.1136/bjsports-2018-099878
Louw A, Diener I, Butler DS, Puentedura EJ. (2011) The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Archives of Physical Medicine and Rehabilitation 92(12):2041-56. https://doi.org/10.1016/j.apmr.2011.07.198
Louw A., Zimney K., Puentedura E.J. and Diener I. (2016) The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract 32(5): 332-355. https://doi.org/10.1080/09593985.2016.1194646
Louw A, Farrell K, Landers M, Barclay M, Goodman E, Gillund J, McCaffrey S. and Timmerman L. (2017) The effect of manual therapy and neuroplasticity education on chronic low back pain: a randomized clinical trial. J Man Manip Ther 25 (5):227-234.https://doi.org/10.1080/10669817.2016.1231860
Malfliet A., Kregel J., Coppieters I., De pauw R., Meeus M., Roussel N., Cagnie B., Danneels L. and Nijs J. (2018) Effect of pain neuroscience education combined with cognition-targeted motor control training on chronic spinal pain: a randomized clinical trial. JAMA Neurol. 75 (7): 808-817. https://doi.org/10.1001/jamaneurol.2018.0492
Moseley, G. L. (2002) “Combined physiotherapy and education is effective for chronic low back pain. A randomised controlled trial.” Australian Journal of Physiotherapy, 48, 297-302.
https://doi.org/10.1016/s0004-9514(14)60169-0
Moseley G.L., Butler D.S. Explain Pain. NOI Group; Adelaide, Australia: 2003.
Moseley G.L., Butler D.S. (2015) Fifteen Years of Explaining Pain: The Past, Present, and Future. J. Pain 16:807–813. https://doi.org/10.1016/j.jpain.2015.05.005
Moseley G.L., Butler D.S. Explain Pain Supercharged. NOI Group; Adelaide, Australia: 2017.
Nijs, J., van Wilgen, C.P., Van Oosterwijck, J., van Ittersum, M. and Meeus, M. (2011). How to explain central sensitization to patients with „unexplained“ chronic musculoskeletal pain : practice guidelines. Man Ther 16(5): 413-418. https:// doi.org/10.1016/j.math.2011.04.005.
Nijs J., Wijma A.J., Willaert W., Huysmans E., Mintken P., Smeets R., Goossens M., van Wilgen P., Van Bogaert W., Louw A., Cleland J. and Donaldson M. (2020) Integrating motivational interviewing in pain neuroscience education for people with chronic pain: a practical guide for clinicians. Phys Ther 1000(5):846-859. https://doi.org/10.1093/ptj/pzaa021
Orhan C., Lenoir D., Favoreel A., Van Looveren E., Kabak V.Y., Mukhtar N.B., Cagnie B. and Meeus M. (2019) Culture-sensitive and standard pain neuroscience education improves pain, disability, and pain cognitions in first-generation Turkish migrants with chronic low back pain: a pilot randomized controlled trial. Physiother Theory Pract 37 (5): 633-645. https://doi.org/10.1080/09593985.2019.1639231
Robins H., Perron V., Heathcote L.C., and Simons L.E. (2016) Pain neuroscience education: state of the art and application in paediatrics. Children (Basel) 3 (4):43. https://doi.org/10.3390/children3040043
Thompson K., Johnson M.I., Milligan J. and Briggs M. (2022) Rethinking pain education from the perspectives of people experiencing pain: a meta-ethnography to inform physiotherapy training. BJM Open 12:e046363. https://doi.org/10.1136/bmjopen-2020-046363
Traeger A.C., Lee H., Hübscher M., Skinner I.W., Moseley G.L., Nicholas M.K., Henschke N., Refshauge K.M., Blyth F.M., Main C.J., Hush J.M., Lo S. and McAuley J.H. (2019) Effect of intensive pain education vs placebo patient education on outcomes in patients with acute low back pain: a randomized clinical trial. JAMA Neurol 76(2): 161-169. https://doi.org/10.1001/jamaneurol.2018.3376
Wood L, Hendrick P.A. (2019) A systematic review and meta-analysis of pain neuroscience education for chronic low back pain: Short-and long-term outcomes of pain and disability. Eur J Pain (United Kingdom) 23(2):234–49. https://doi.org/10.1002/ejp.1314

.jpg)


Comments